Editor’s Note:
The 18th World Conference of Lung Cancer (WCLC), hosted by International Association for the Study of Lung Cancer (IASLC), was held from October 15th–18th in Yokohama, Japan. It’s our great pleasure to have a brief interview with Dr. Peter Ujhazy.
Dr. Peter Ujhazy: research for the greater good
Expert Introduction
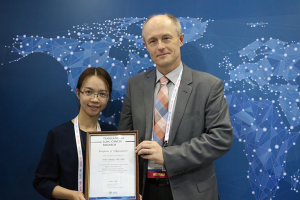
Peter Ujhazy (Figure 1) is the Deputy Associate Director of the Translational Research Program, Division of Cancer Treatment and Diagnosis at the National Cancer Institute.
He has received his Medical Degree at the Comenius University, and his PhD at the Cancer Research Institute of the Slovak Academy of Sciences in Bratislava, Czechoslovakia, where he started his career in the Department of Tumor Immunology.
He was involved in the development of diagnostics in blood malignancies, he studied natural immunity in lymphoid malignancies, and gained clinical experience in the adjacent Cancer Center.
He worked for 6 years as a Visiting Scientist and later as a Cancer Research Scientist in Dr. Henry Mihich’s laboratory at Roswell Park Cancer Institute in Buffalo, NY, USA and published extensively on chemo-immunotherapy and multidrug resistance.
After a short stay in the biotech company Biotech Research Laboratories in the Washington, DC metropolitan area, he decided not to pursue a career in industry and accepted a position in Dr. Irvin Arias’ laboratory in the Department of Physiology, Tufts University in Boston, MA, where he studied the physiologic role of ATP-dependent transporters.
In 2001, Dr. Ujhazy accepted a position in the National Cancer Institute’s Organ Systems Branch that managed Specialized Programs of Research Excellence (SPOREs). Working with SPOREs grants brought him closer to the ultimate goal of his original training—that is to help patients and populations at risk of cancer.
Over the past 14 years, Dr. Ujhazy has served as the Program Director for Lung, Leukemia, Lymphoma, Myeloma, Sarcoma, GI, Pancreas, Head & Neck, and Brain Tumor SPOREs. Currently, he is in charge of SPOREs in Lung cancer, Myeloma, and Sarcoma. His other duties include serving on various NCI committees and working groups.
Interview (Figure 2)

Dr. Peter Ujhazy gave a speech entitled “NCI’s Small Cell Lung Cancer Consortium: New Answers to Old Questions”. He shared with us more about the priorities in small cell lung cancer (SCLC) research, his enthusiasm about the projects involved in the National Cancer Institute (NCI) consortium, and some advice for young investigators in the field.
Dr. Ujhazy said that the National Cancer Institute (NCI) of the United States of America, where he comes from, convened in 2013 and 2014 with a large group of international scientists to answer a very simple question that had a very complex answer, which is “what are the priorities in SCLC research?” There are five priorities that they designated, and he believes these priorities still hold true today:
- Development of better research tools for the study of SCLC;
- Conduct of comprehensive genomic profiling of SCLC;
- Creation of new diagnostic and prevention approaches for SCLC;
- Therapeutic development efforts;
- Study of mechanisms underlying both high rate of initial response and rapid emergence of drug and radiation resistance.
He said those would be the five priorities that are important for investigators and clinicians even today.
As one of the leading experts in NCI SCLC consortium, Dr. Ujhazy also shared with us the research projects undertaken:
- The first project, led by Drs. Serge Nana-Sinkam from Virginia Commonwealth University and James Lee from Ohio State University attempts to carry out an analysis of nucleic acids found in exosomes using molecular beacons contained on biochips to detect specific mRNA and miRNA sequences. The ultimate goal is to design an early diagnostic test;
- The second project is led by Dr. Samir Hanash at University of Texas MD Anderson Cancer Center and it dwells on proteomic and autoantibody-based prognostic tests from blood that would allow detecting SCLC in high risk populations before other screening tests;
- The third project is conducted by Dr. John Thomas Poirer (Sloan Kettering Institute for Cancer Research) and it builds on the earlier clinical success of the antibody-drug conjugate against a ligand of the Notch pathway, DLL3, selectively expressed on the surface of SCLC cells;
- The fourth project designed by Drs. Kwok Kin Wong from New York University and Nathanael Schiander Gray from Dana-Farber Harvard Cancer Institute aims to define transcriptional and epigenetic factors that contribute to chemotherapy-resistance in both tumor cells and the surrounding microenvironment and assess the efficacy of transcriptional CDK inhibitors alone or in combination with novel investigational therapies, utilizing in vivo SCLC models;
- The fifth project is led by Drs. John Heymach, Lauren Byers (both from the University of Texas MD Anderson Cancer Center), and Julien Sage from Stanford University. The investigators seek to identify improved treatment strategies in SCLC using immunotherapeutic agents targeting the PD1 pathway;
- The sixth project is at University of Texas Southwestern led by Dr. Minna. They are looking also at therapeutic targets, however, they focus on two defining molecules that basically define the neuroendocrine nature of SCLC. ASCL1 is one of them, and NEUROD1 is the other.
It’s important to seek advice along the path of a research career, and I do have some suggestions to offer. At the end of the interview, as an experienced expert, Dr. Ujhazy gave some suggestions to young researchers.
“It is extremely important in science, perhaps more than in other fields, that the data one produces are reproducible and solid. We know science moves forward and there may be future discoveries that may contribute to or expand on the knowledge we have, but those discoveries need to stand on a solid base. My suggestion to young investigators would be to not hesitate to go ahead to ask tough questions, but once they have some data that they believe is strong data, to verify even more than what they think is necessary, and look at them from different angles. So that once the data is published in the public domain, there is no doubt that the data is solid. Unfortunately, in many situations, while it may not be caused by one’s mistake or neglect, it’s possible that not all the questions were asked and answered, and what happens is that there is a published paper out there, but no one can reproduce the data.
The other thing I would like to suggest especially to PhD scientists working in the lab is: whatever your focus is, try to get in touch with clinicians who have the clinical questions. I’m coming from a translational culture—we sponsor translational research. While basic research is pivotal and there are some questions that are being answered today, but their clinical utilisation will be in the far future maybe 10–20 years from now; it’s always good to know what the current clinical needs are, and to modify your research accordingly. If you don’t do that, for example, you may be working for 2 years on something you feel is really important to the field, and once you speak to the clinician, they tell you ‘this is nice, but we have other means to handle this’, and that makes your work redundant.
I would try to always check, whether what we’re working on is relevant now or in the future, with a clinical situation, because ultimately, we do all this research not only because we want to understand what’s going on in the biology of the disease, but because we want to use this knowledge for the greater good. We want the patients to be able to benefit from it, or even better, if we can prevent the disease wholly, that makes our work more meaningful.”
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Poon B, Liu M. Dr. Peter Ujhazy: research for the greater good. Asvide 2017;4:578. Available online: http://www.asvide.com/articles/1900
(Science Editor: Bella Poon, Macy Liu, TLCR, tlcr@amepc.org)