Coronary artery calcification in lung cancer screening
Introduction
Lung cancer screening has been shown in the National Lung Screening Trial (NLST) to result in a statistically significant decrease in lung cancer specific mortality (1). In addition to the lung cancer specific mortality reduction, there was a statistically significant 7% reduction in all-cause mortality. As the entirety cannot be explained simply by lung cancer mortality reduction, it is conceivable that the detection of abnormalities incidentally detected during a screening CT might be playing a role.
The effects of smoking extend beyond lung cancer, and smokers are also at risk for premature deaths due to chronic obstructive pulmonary disease (COPD), heart disease and stroke. For subjects in the lung cancer screening window, the relative risk of death due to ischemic heart disease is greater than 3 times that of a non-smoker (2). Moreover, smoking reduces the time to development of coronary artery calcium (up to 10 years earlier for current smokers) when compared with non-smokers (3). As the risk for cardiovascular deaths decreases in former smokers, there is the opportunity for two teachable moments. The first is the ability to teach screening subjects about the benefit of smoking cessation for cardiovascular risks, and the second is the ability to provide counselling for both current and former smokers on their current cardiovascular risks, which can lead to further lifestyle changes or improved pharmacological management.
Cardiac risk factors as defined by the Framingham Heart Study (FHS) include not only age and smoking, but also systolic blood pressure, total cholesterol, high density-lipoprotein (HDL) and body mass index (BMI) (4). Without any other risk factors, smokers already fall into the low end of intermediate risk. While risk factor information could be obtained and counseling performed at a lung cancer screening visit, the screening CT provides equally if not more important prognostic information.
The ability to detect and quantify coronary artery calcification on CT has been around since the early 1990’s (5). The most widely used system is that developed by Agatston with coronary calcium defined as a lesion greater than 130 Hounsfield units with an area of at least 1 mm2. The score is derived based on maximal density and is typically obtained by circling the suspect lesions and calculating the score via a computer algorithm. Risk can then be stratified by overall scores with a score of zero indicating absence of calcified plaque, 1–10 minimal plaque, 11–100 mild plaque, 101–400 moderate plaque, and >400 severe plaque (5). Although there is inherent inter-scan variability in scores, the numerical groupings hold up well and thus are more important than the exact ordinal score. Volume scores can also be obtained. Volume scores tend to be more reproducible and better suited for longitudinal follow up (6) but are seldom used, particularly since electron beam CT scanners have fallen out of favor.
Calcium in the coronary arteries therefore is an imaging biomarker for the presence of coronary artery atherosclerosis and can play a role in the primary prevention of coronary heart disease (CHD) (7). Although classically detected on cardiac gated CTs, calcium in the coronary arteries can be detected on non-gated studies without intravenous contrast and at low radiation doses. This makes screening CTs an excellent target for determining cardiac risks without additional radiation. In this review we will discuss the use of coronary artery calcium scoring for the detection of atherosclerotic disease and its potential application to lung cancer screening populations.
Significance of CT-detected coronary artery calcium
In nearly all prognostic trials, the presence of coronary artery calcium has proven to be a reliable biomarker for cardiovascular events and portends risk better than other clinical criteria. The Multi-ethnic Study of Atherosclerosis (MESA) study enrolled 6,814 individuals and followed them for over 3 years (8). In the overall population, the prevalence of a non-zero score was highest for white males (70.4%), while the corresponding rate for white females was 44.7%. There was a statistically significant lower prevalence in African-American, Hispanic and Chinese individuals of both genders. Compared to a calcium score of zero, hazard ratios for major adverse cardiac events (MACE), including myocardial infarct and coronary related death was 3.89 for a score of 1–100, 7.08 for a score of 101–300, and 6.84 for a score of >300. The corresponding hazard ratios for any coronary events were 3.61, 7.78, and 9.67, respectively. Overall a doubling of calcium score was associated with a 20% increase in risk. The presence of a zero calcium score is equally important as it confers a very low risk of coronary events (1.1–1.7%) over 10 years regardless of the presence of traditional risk factors (9).
Equally important is the correlation between calcium score and FHS risk factors, where a calcium score ranging from 101–400 carries the same risk as an intermediate Framingham risk with an associated 10-year risk of coronary events ranging from 12.8–16.4% (7). Coronary calcium can also be used to reclassify coronary risks defined by FHS. Adding calcium score resulted in a reclassification of risk group in 26% of the MESA population (10). In the intermediate risk group, calcium scores reclassified 16% to a higher risk group and 39% to a lower risk group. As such, coronary calcium has the ability to better classify cardiac risk in a population of smokers. This reclassification ability is particularly valuable in patients with intermediate Framingham risk, in which management guidelines are less well-defined than cases of low or high risk. Caution should be made in the interpretation of a zero calcium score, as smokers with a zero score have similar all-cause mortality to non-smokers with mild to moderate atherosclerosis (11).
Methods of interpretation
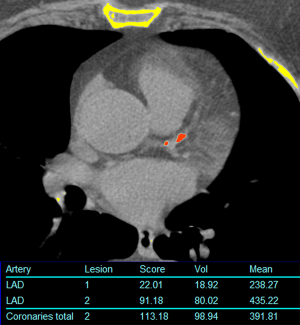
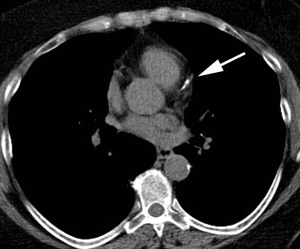
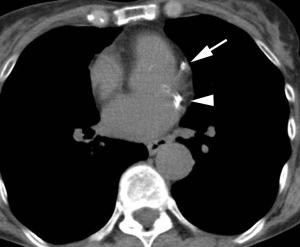
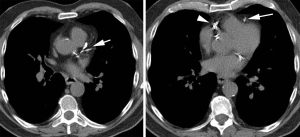
Computer aided calculation of Agatston score is the most commonly used technique for calculation of the calcium score. Automated or semi-automated workflows identify and compile coronary artery calcium plaques >130 HU into a single numerical score (Figure 1). There is excellent inter- and intra-observer agreement in quantitative measures (12). Because this may need to be calculated at a separate workstation and not directly validated for non-gated studies, other systems have been developed to provide a qualitative measure of coronary artery calcium. One method is to use ordinal scores for each of the four major coronary arteries [left main, left anterior descending (LAD), circumflex (LCX), and right coronary artery (RCA)] assigning a score from 0–3 based on the severity of disease in each one resulting in an overall score between 0–12. A simpler method is to simply analyze the entire coronary artery system as a single unit resulting in an overall “gestalt” of disease severity summarized as absent, mild, moderate, or heavy (Figures 2-4). Comparative studies vary in terms of which scoring methods are used.
Gated versus non-gated CT for detection of coronary artery calcium
As calcium scoring evolved as a gated technique, there have been questions as to whether a non-gated study is sufficient to assign risk. While gated CT has been the gold standard for coronary artery quantification, there is compelling evidence that this can be ascertained using non-gated studies of the chest as well. In a retrospective study of 410 patients, the presence of coronary artery calcium was shown to be a strong independent predictor for myocardial infarct and all-cause mortality (13). In a nested case control study of over 4,500 individuals, 3 mm gated CT Agatston scores were compared with same day 6 mm non-gated Agatston scores. Not unexpectedly, scores were systematically lower on the thicker sections of the non-gated studies (due to volume averaging and hence underestimation). Despite this, there was a strong correlation with increasing calcium scores and mortality (14). The latter study suggests that if Agatston scores are to be used on non-gated studies with thicker collimation, new lower risk thresholds may need to be established. The variability is lower when similar slice thickness is utilized but still results in a mean variability of approximately 44% (15). Improvements can further be made by using high pitch techniques, resulting in less than 2% variance in calcium score (16). A meta-analysis combing both lung cancer screening and routine studies from a variety of sources found that non-gated CT underestimated calcium score in 19% and overestimated calcium in 2.6% relative to a gated Agatston score of 400 (17).
In 222 individuals who underwent same day gated and non-gated CT of the chest, the use of Agatston score was compared to an ordinal scale. Ordinal scores of 1–3, 4–5, and ≥6 corresponded to average Agatston scores of 98.7, 350.6 and 1,925 respectively (18). Similarly, Kirsch et al. found that an ordinal score of >2 correlated with a calcium score of >100 (AUC =0.976) and an ordinal score of >7 reliably detected a calcium score of >400 (AUC =0.991) (19). In this manner, ordinal scores can be used to predict low, intermediate and high risk individuals. Ordinal scoring has also been shown to have excellent correlation with Agatston scores in subjects with acquired immunodeficiency syndrome (AIDS) (20). While the data supporting the use of non-gated calcium scores in routine practice remains somewhat controversial, there is an abundance of data in lung cancer screening populations.
Coronary calcium in lung cancer screening trials
Asia
There have been four publications related to coronary artery calcification and lung cancer screening in institutions from Asia. Notably, none of these publications evaluate the correlation of coronary calcium with cardiovascular morbidity and mortality. The prevalence and distribution of coronary calcium have been described in Japan (21). In a cohort of 1,834 lung cancer screening studies, a non-zero calcium score was detected in 26.9% of all subjects. Similar to other populations, calcium was more prevalent in males (29.8%) compared with females (17.1%).
In China, one study enrolled 401 subjects who underwent both lung cancer screening and gated CT for Agatston score (22). Coronary calcium was detected on the gated CT in 146 (39.6%) with a false negative rate of 1.9% for detecting calcium on the screening CT in subjects with a calcium score ≥10. A scoring system using a 4-point scale (absent, mild, moderate, severe) had a high concordance with Agatston score risk categories (k=0.813). A similar study performed in Korea investigated 117 subjects with a positive calcium score who underwent lung screening (23). In this study, visual scores also had a high degree of association, with 71.6% of visual scores falling into the same risk category and 98.9% varying by no more than one risk category.
A study including 128 Korean subjects compared screening CT reconstructed at 1, 2.5 and 5 mm thickness and calcium thresholds of 90 and 130 HU to standard Agatston scores derived from gated CT (24). Sensitivity for detection of any calcium was best with 1 mm slice thickness and a calcium threshold of 130 HU as well as 2.5 mm slice thickness with a calcium threshold of 90 HU. With regards to accuracy, scans with 2.5 mm slice thickness and calcium threshold of 130 HU provided the best correlation with the reference standard (r=0.89).
Europe
There have been numerous publications related to coronary artery calcification and lung cancer screening in institutions from Europe. A 60 subject feasibility study showed that while overall calcium scores were higher for gated CT, the correlation of the values from screening CT was high (r=0.98) (25). The reclassification rate was 38%, typically to a lower risk group on the screening CT. Notably, the radiation dose for the screening CT was approximately 25% lower than gated CT. Visual analysis has been shown to correlate with Agatston scores in European populations (26).
There have been several studies from the Dutch-Belgium Randomized Lung Cancer Screening Trial (NELSON) assessing the prognostic value of non-gated calcium score for mortality and cardiovascular events. The largest patient group involved 3,111 males who underwent 2.9 years of follow-up with a total of 186 cardiovascular events (27). The investigators chose to use a modified Agatston score and strata with scores of 1–10, 10–100, 100–400, and >400 with adjusted hazard ratios (HRs) of 3.39, 6.52, 6.58, and 12.58. Adding calcium volume and number of calcifications improved classification of risk, but not nearly as strongly as Agatston score. In a related study spirometric parameters were also associated with cardiovascular events but did not contain independent prognostic information (28).
In a case cohort design, 958 asymptomatic individuals from the NELSON Trial were evaluated including 150 cases where either a cardiovascular event or death occurred and 808 control subjects (29). Agatston scores were acquired from the non-gated CT and assigned to traditional risk groups. Mortality was related to increasing calcium scores and ranged from 0.08% for no calcium to 1.1% for subjects with a calcium score >1,000. Compared to calcium scores of zero, HR for mortality for scores of 1–100; 101–1,000 and >1,000 were 2.82, 5.96 and 10.24. Corresponding HR for cardiovascular events were 1.38, 3.04 and 7.77 when adjusting for other cardiac risk factors such as hypertension. In the intermediate and high risk groups, 48–64% of subjects were not treated with statin based therapy, demonstrating a role for improved primary prevention of cardiovascular events in a lung cancer screening population.
Finally, two separate screening centers (derivation and validation cohorts) have been used to create a prediction model for cardiovascular events in males (30). Similar to the case-cohort study, HR increased for cardiovascular events with increasing calcium score. In addition, they showed that a model that included age, cardiovascular history, smoking status, cigarette pack years, coronary calcium volume and aortic calcium volume could subdivide individuals into non- high and high risk groups (less than/greater than 6% event rate at 3 years).
Agatston scores were measured in 1945 participants in the Danish Lung Cancer Screening trial (DLCST) (31). Survival rates were 98%, 96% and 92% for calcium scores of 0, 1–400, and >400 respectively. In addition, the HR for cardiovascular deaths was 3.8 for calcium scores >400. A calcium score of >400 was independently associated with both all-cause mortality [odds ratio (OR) =3.73] and cardiovascular events (OR =2.87) in the Multicentric Italian Lung Detection (MILD) trial (32). In addition, calcium score was found to be a better predictor of cardiovascular events and all-cause mortality in this screening population than either emphysema or forced expiratory volume in 1 second (FEV1).
North America
The associations of coronary artery calcium and outcomes have been studied both in the non- randomized Early Lung Cancer Action Project (ELCAP) and NLST. In the ELCAP, the ordinal scoring was used in 8,782 smokers age 40–85 with an increasing risk of cardiovascular death occurring with an increasing ordinal score: 1.2% with a score of zero, 1.8% with a score of 1–3, 5.0% for a score 4–6, and 5.3% for a score ≥7 (33). They noted that coronary calcium remained the most important factor after adjusting for age, gender and smoking pack years.
Similar information has been derived from the NLST. In the Lung Screening Study arm 1,000 participants who died were matched 1:1 by age, smoking pack years and CT scanner type (34). This study used both the ordinal scoring system and a visual score based on linear extent and thickness of calcification. The presence of any calcium was associated with a 3-fold increase in cardiovascular deaths and increasing risk associated with increasing score. While there was better inter-observer agreement for the visual score, the ordinal score showed a slightly better fit in risk prediction.
In the American College of Radiology Imaging Network (ACRIN) arm of the NLST, a random sample of 1,575 cases included 210 cardiovascular deaths, 315 deaths from other causes and 1,050 that were alive at the end of the trial (35). For this study, three scoring systems were used: the Agatston score, the vessel based scoring system and an overall “gestalt” as to whether overall calcium was absent, mild, moderate, or heavy. Compared to a calcium score of zero, all scoring methods showed an increasing risk of cardiovascular death with increasing score. For Agatston scores of 1–100, 101–1,000, and >1,000 the HR was 1.27, 3.57 and 6.63, respectively, while using a simple overall gestalt resulted in a HR of 2.09 for mild, 3.86 for moderate, and 6.95 for severe. The implication of this is that more time-consuming scoring systems do not necessarily result in better risk prediction and that this may simplify reporting of the severity of coronary artery atherosclerosis in clinical practice.
Conclusions and recommendations
Coronary calcium is a valuable imaging biomarker for the presence of atherosclerotic disease and the prediction of cardiovascular events. Ample research has shown that, similar to gated CT scans, non-gated CT can play a comparable role in diagnosis and risk prediction. This has been further carried over to the lung cancer screening population where increasing qualitative and quantitative scores are associated with greater cardiac events and cardiac related deaths. Therefore, lung cancer screening provides a teachable moment for both lung and cardiovascular health and should be considered an important part of the discussion of CT findings with patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med 2013;368:351-64. [Crossref] [PubMed]
- Lehmann N, Mohlenkamp S, Mahabadi AA, et al. Effect of smoking and other traditional risk factors on the onset of coronary artery calcification: results of the Heinz Nixdorf recall study. Atherosclerosis 2014;232:339-45. [Crossref] [PubMed]
- D'Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008;117:743-53. [Crossref] [PubMed]
- Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827-32. [Crossref] [PubMed]
- Callister TQ, Cooil B, Raya SP, et al. Coronary artery disease: improved reproducibility of calcium scoring with an electron-beam CT volumetric method. Radiology 1998;208:807-14. [Crossref] [PubMed]
- Hecht HS. Coronary artery calcium scanning: past, present, and future. JACC Cardiovasc Imaging 2015;8:579-96. [Crossref] [PubMed]
- Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008;358:1336-45. [Crossref] [PubMed]
- Nasir K, Rubin J, Blaha MJ, et al. Interplay of coronary artery calcification and traditional risk factors for the prediction of all-cause mortality in asymptomatic individuals. Circ Cardiovasc Imaging 2012;5:467-73. [Crossref] [PubMed]
- Polonsky TS, McClelland RL, Jorgensen NW, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2010;303:1610-6. [Crossref] [PubMed]
- McEvoy JW, Blaha MJ, Rivera JJ, et al. Mortality rates in smokers and nonsmokers in the presence or absence of coronary artery calcification. JACC Cardiovasc Imaging 2012;5:1037-45. [Crossref] [PubMed]
- Yamamoto H, Budoff MJ, Lu B, et al. Reproducibility of three different scoring systems for measurement of coronary calcium. Int J Cardiovasc Imaging 2002;18:391-7. [Crossref] [PubMed]
- Shao L, Yan AT, Lebovic G, et al. Prognostic value of visually detected coronary artery calcification on unenhanced non-gated thoracic computed tomography for prediction of non-fatal myocardial infarction and all-cause mortality. J Cardiovasc Comput Tomogr 2017;11:196-202. [Crossref] [PubMed]
- Hughes-Austin JM, Dominguez A 3rd, Allison MA, et al. Relationship of Coronary Calcium on Standard Chest CT Scans With Mortality. JACC Cardiovasc Imaging 2016;9:152-9. [Crossref] [PubMed]
- Budoff MJ, Nasir K, Kinney GL, et al. Coronary artery and thoracic calcium on noncontrast thoracic CT scans: comparison of ungated and gated examinations in patients from the COPD Gene cohort. J Cardiovasc Comput Tomogr 2011;5:113-8. [Crossref] [PubMed]
- Hutt A, Duhamel A, Deken V, et al. Coronary calcium screening with dual-source CT: reliability of ungated, high-pitch chest CT in comparison with dedicated calcium-scoring CT. Eur Radiol 2016;26:1521-8. [Crossref] [PubMed]
- Xie X, Zhao Y, de Bock GH, et al. Validation and prognosis of coronary artery calcium scoring in nontriggered thoracic computed tomography: systematic review and meta-analysis. Circ Cardiovasc Imaging 2013;6:514-21. [Crossref] [PubMed]
- Azour L, Kadoch MA, Ward TJ, et al. Estimation of cardiovascular risk on routine chest CT: Ordinal coronary artery calcium scoring as an accurate predictor of Agatston score ranges. J Cardiovasc Comput Tomogr 2017;11:8-15. [Crossref] [PubMed]
- Kirsch J, Buitrago I, Mohammed TL, et al. Detection of coronary calcium during standard chest computed tomography correlates with multi-detector computed tomography coronary artery calcium score. Int J Cardiovasc Imaging 2012;28:1249-56. [Crossref] [PubMed]
- Chandra D, Gupta A, Leader JK, et al. Assessment of coronary artery calcium by chest CT compared with EKG-gated cardiac CT in the multicenter AIDS cohort study. PloS One 2017;12:e0176557. [Crossref] [PubMed]
- Ohmoto-Sekine Y, Yanagibori R, Amakawa K, et al. Prevalence and distribution of coronary calcium in asymptomatic Japanese subjects in lung cancer screening computed tomography. J Cardiol 2016;67:449-54. [Crossref] [PubMed]
- Huang YL, Wu FZ, Wang YC, et al. Reliable categorisation of visual scoring of coronary artery calcification on low-dose CT for lung cancer screening: validation with the standard Agatston score. Eur Radiol 2013;23:1226-33. [Crossref] [PubMed]
- Kim YK, Sung YM, Cho SH, et al. Reliability analysis of visual ranking of coronary artery calcification on low-dose CT of the thorax for lung cancer screening: comparison with ECG-gated calcium scoring CT. Int J Cardiovasc Imaging 2014;30 Suppl 2:81-7. [Crossref] [PubMed]
- Kim SM, Chung MJ, Lee KS, et al. Coronary calcium screening using low-dose lung cancer screening: effectiveness of MDCT with retrospective reconstruction. AJR Am J Roentgenol 2008;190:917-22. [Crossref] [PubMed]
- Arcadi T, Maffei E, Sverzellati N, et al. Coronary artery calcium score on low-dose computed tomography for lung cancer screening. World J Radiol 2014;6:381-7. [Crossref] [PubMed]
- Dirrichs T, Penzkofer T, Reinartz SD, et al. Extracoronary Thoracic and Coronary Artery Calcifications on Chest CT for Lung Cancer Screening: Association with Established Cardiovascular Risk Factors - The "CT-Risk" Trial. Acad Radiol 2015;22:880-9. [Crossref] [PubMed]
- Takx RA, Isgum I, Willemink MJ, et al. Quantification of coronary artery calcium in nongated CT to predict cardiovascular events in male lung cancer screening participants: results of the NELSON study. J Cardiovasc Comput Tomogr 2015;9:50-7. [Crossref] [PubMed]
- Takx RA, Vliegenthart R, Mohamed Hoesein FA, et al. Pulmonary function and CT biomarkers as risk factors for cardiovascular events in male lung cancer screening participants: the NELSON study. Eur Radiol 2015;25:65-71. [Crossref] [PubMed]
- Jacobs PC, Gondrie MJ, van der Graaf Y, et al. Coronary artery calcium can predict all-cause mortality and cardiovascular events on low-dose CT screening for lung cancer. AJR Am J Roentgenol 2012;198:505-11. [Crossref] [PubMed]
- Mets OM, Vliegenthart R, Gondrie MJ, et al. Lung cancer screening CT-based prediction of cardiovascular events. JACC Cardiovasc Imaging 2013;6:899-907. [Crossref] [PubMed]
- Rasmussen T, Kober L, Abdulla J, et al. Coronary artery calcification detected in lung cancer screening predicts cardiovascular death. Scand Cardiovasc J 2015;49:159-67. [Crossref] [PubMed]
- Sverzellati N, Cademartiri F, Bravi F, et al. Relationship and prognostic value of modified coronary artery calcium score, FEV1, and emphysema in lung cancer screening population: the MILD trial. Radiology 2012;262:460-7. [Crossref] [PubMed]
- Shemesh J, Henschke CI, Shaham D, et al. Ordinal scoring of coronary artery calcifications on low-dose CT scans of the chest is predictive of death from cardiovascular disease. Radiology 2010;257:541-8. [Crossref] [PubMed]
- Watts JR Jr, Sonavane SK, Snell-Bergeon J, et al. Visual scoring of coronary artery calcification in lung cancer screening computed tomography: association with all-cause and cardiovascular mortality risk. Coron Artery Dis 2015;26:157-62. [Crossref] [PubMed]
- Chiles C, Duan F, Gladish GW, et al. Association of Coronary Artery Calcification and Mortality in the National Lung Screening Trial: A Comparison of Three Scoring Methods. Radiology 2015;276:82-90. [Crossref] [PubMed]


