State of the art in surgery for early stage NSCLC—does the number of resected lymph nodes matter?
Introduction
Surgery is the treatment of choice in patients with early stage NSCLC. However, results remain poor in these patients, with 5-year survival rates ranging from 84% in stage I to 39% in stage IIIA, according to different studies (1).
The heterogeneity of patients in different stages and errors in staging may be related to these differences in survival.
Lymph node involvement is the main prognostic factor in patients with NSCLC, but there is still no clear definition of the number of nodes required to consider a lymphadenectomy as complete.
The objective of this article is to review the published literature presented at the 10th Congress on Lung Cancer of the Spanish Lung Cancer Group, in Barcelona, November 2013.
Lymph node involvement
Mediastinal lymph node involvement is the main prognostic factor in patients with NSCLC, and therefore one of the goals of surgical treatment is to diagnose such involvement and establish accurate staging to provide the patient with proper treatment. One of the aims of lymph node dissection, both hilar and mediastinal, is to achieve an intraoperative staging as accurate as possible, and to obtain local control of the disease (2).
There is an ongoing debate about the extent to which a lymphadenectomy procedure can be performed in patients with stage I lung cancer. During the procedure, the surgeon can choose between different procedures: from not removing any nodes, to performing a non-systematic sampling or carrying out a bilateral complete mediastinal dissection, as is done by some Japanese teams (3,4). Only the pathologist can say what nodes are affected and detect the presence of micrometastases. The characteristics of the nodes, whether they are calcified for example, can determine the surgeon’s attitude regarding what technique to choose, but, as Gaer and Goldstraw (5) proved, it is not possible to predict intraoperatively which lymph node will be affected based on its appearance. In 68% of patients in the series published by Takizawa, the surgeon was not able to determine whether the mediastinal nodes were involved or not because their macroscopic appearance was normal (6). In the series of Riquet, 20% of the positive nodes were perceived as possible negative by the surgeon, proving that ocular assessment is inexact (7). It is proved that non-systematic sampling is not reliable for proper staging (8,9).
Minimum number of lymph nodes
Unlike in lung cancer, in other tumors there does exist a defined number of nodes required to consider a lymphadenectomy as complete. In the case of colorectal cancer, survival has a direct relationship between the number of lymph nodes examined (10). Several authors have shown that twelve is the minimum number of lymph nodes needed to stage a patient as N0 (11,12). The American Society of Clinical Oncology (ASCO) recommends treatment with adjuvant chemotherapy for all patients staged as N0 with less than 12 lymph nodes resected, since they are at high risk of recurrence (13).
In lung cancer, the minimum number of lymph nodes necessary to consider a lymphadenectomy as complete is not clearly defined. Some authors have tried to state this in several studies. Doddoli considered a lymphadenectomy as complete when more than ten lymph nodes from at least two different mediastinal levels were removed (14). Wu et al. considered a lymphadenectomy as inadequate for proper staging and local control of the disease if less than 15 lymph nodes had been resected (15).
Guidelines recommendations
Although there is no defined minimum number of lymph nodes for a complete lymphadenectomy, there are some recommendations for performing this procedure published by different scientific societies. Thus, the European Society of Thoracic Surgeons (ESTS) recommends systematic nodal dissection in all cases (16). Ideally, this should be done as an en bloc resection of the upper mediastinal nodes on the right side stations (2R and 4R), any visible nodes stations 3a and 3p, and the lower mediastinum, (stations 7, 8, and 9). On the left side, removal of stations 5 and 6, and inferior paratracheal (4L) lymph nodes is minimally required. For a complete nodal dissection of the left upper mediastinum, it is recommended to perform a division of the ligamentum arteriosus allowing mobilization of the aortic arch. In addition, it is important that the highest mediastinal node removed should be identified, in order to assess whether the resection is complete (16).
For peripheral squamous T1 patients, a lobe-specific systematic nodal dissection is acceptable, if the hilar and interlobar lymph nodes are negative, because it has been shown that the probability of unforeseen N2 disease is very low (<5%) in such patients. In this case, it is necessary to remove three mediastinal stations, always including station 7, and at least six lymph nodes must be excised (16).
Common practice in thoracic surgery
Current practice in thoracic surgery regarding lymphadenectomy differs on some points to the guideline recommendations. A survey of surgeons in the UK revealed that 45% of them did not perform sampling if mediastinal nodes had a normal macroscopic appearance, and only 23% of them performed routine complete lymphadenectomy (17).
In another survey conducted in 2001 to examine patterns of treatment of 11,000 patients with NSCLC, the authors observed that 42.2% of the patients did not undergo any type of lymph node dissection (18).
Analysis of the Society of Thoracic Surgeons’ database also showed similar data, with no mediastinal lymph node evaluation in 35% of patients (19).
More recently, two papers continue to show similar practices. The review of the SEER database confirmed that 48% of patients had no assessment of mediastinal lymph nodes (20), and a retrospective cohort study in the Netherlands in 216 patients, demonstrated that no lymphadenectomy was performed in 21 patients with suspicious mediastinum by CT scan or PET-CT (21). This series also showed that only eight patients met ESTS criteria (21).
The more lymph nodes resected, the more positive lymph nodes identified
It seems obvious, from a logical point of view, to think that the probability of finding a positive node increases with the number of lymph nodes analyzed. This was proved in the Izbicki series, in which a complete lymphadenectomy increased the percentage of patients in whom positive mediastinal lymph nodes were detected (22).
Comparing complete lymphadenectomy to sampling, Bollen et al. showed that more positive lymph nodes can be diagnosed with complete lymphadenectomy (35%) than with sampling (13%), concluding that sampling is inadequate for accurate staging (23). Similar data were found by Keller et al. (24).
In the papers published by Naruke et al. (25) and Yoshino et al. (26), the results are similar: sampling detected between 9% and 17% of positive nodes, and complete lymphadenectomy obtained between 22% and 32% positive lymph nodes.
In a review of patients operated on in our department in Vall d’Hebron University Hospital, Barcelona, similar data were found, with a greater number of positive nodes in the group of patients with more than ten lymph nodes resected (27) (Table 1).
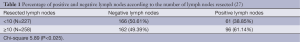
Full table
Therefore, a complete lymphadenectomy provides proper staging which helps to identify patients’ real prognosis. Hence, professionals are able to offer appropriate treatment according to the patient’s stage.
The more lymph nodes resected, the better the survival
Several nonrandomized studies and retrospective series have shown that survival increases in the group of patients with a higher number of lymph nodes removed.
Wu et al. published a series of 471 patients with stage I-IIIA NSCLC, comparing complete lymphadenectomy to systematic sampling. They observed that 5-year survival in the sampling group was 36.98%, compared to 48.37% in the lymphadenectomy group (statistically significant difference) (28).
In our data, the results were similar, identifying the number of nodes as a protective factor in the multivariate analysis (27) (Table 2).
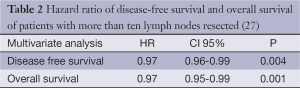
Full table
In two articles published by Lardinois et al. (29) and Sakurai et al. (30), no significant difference in overall survival was observed between lymphadenectomy and sampling, but there was an increase in disease-free survival and in local recurrences if patients underwent complete lymphadenectomy.
A recent meta-analysis of three studies observed a benefit in survival in stage I, II and IIIA patients if lymphadenectomy was complete, and that this procedure reduced the risk of death in early stages (31).
Complete lymphadenectomy in stage I NSCLC patients
The improvement in survival in early stages is also seen in the series published by Wu et al., with 5-year survival of 57.49% in the sample group compared to 82.16% if complete lymphadenectomy was performed (27).
In another study published in 2003 in which 321 stage I patients were analyzed, 5-year survival was significantly higher in the group with more than 15 lymph nodes resected (57.1% vs. 54.5%), concluding that the number of lymph resected could explain the differences in survival in stage I patients (15).
In a review of 442 stage I patients, those in whom less than six nodes were resected through lymphadenectomy showed higher recurrence and mortality rates than the group with complete lymphadenectomy (32).
Similar data were observed in a paper published by Ou et al., analyzing stage IA patients. They found a 5-year survival rate of 75.9% in the group with more than 15 resected lymph nodes, compared to 57.9% in the group with less than 6 resected lymph nodes (33).
Xu et al. recently published a series of 203 stage IA patients with 5-year overall survival of 62%. They divided the series into three groups according to the number of lymph nodes resected (<10 nodes, 10 to 20, and >20). The analysis of disease-free survival showed statistically significant differences between the groups: 20.26%, 58.8% and 75% respectively. The differences remain significant in the analysis of the number of resected stations, and the data are very striking when analyzing the mediastinal stations resected (9.1% when less than three mediastinal stations were resected vs. 65.1% when more than 3) (34). The authors point out that if an adequate lymphadenectomy is not performed, the true N stage remains unknown, which can result in misclassification of stage IA (33).
In a randomized study comparing sampling vs. complete lymphadenectomy in patients with T1 and T2 N0 or N1 with no hilar involvement, the authors found no differences in long-term survival rate of local or regional recurrence (35). This study did not include patients with nodal involvement of station 10, so the possibility of mediastinal stations may be low, which could explain the results. The authors, however, conclude that a complete lymphadenectomy provides the most accurate staging. They also point out that current preoperative staging cannot accurately identify patients with mediastinal lymph node involvement. Another reason for this procedure is that patients with known hilar or N2 disease, or with T3/T4 tumors, may benefit from mediastinal lymph node dissection. Therefore, the authors still recommend that all patients with resectable NSCLC undergo mediastinal lymph node dissection because the procedure does not increase mortality or morbidity (34).
Conclusions
There is no contraindication for performing a complete lymphadenectomy. The increase in survival in patients with complete lymphadenectomy may be due to more accurate staging. Therefore, complete lymphadenectomy should be mandatory, even in early stage patients.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- LoCicero J III. Surgical Treatment of Non-Small-Cell Lung Cancer. In: Shields TW, LoCicero J III, Reed CE, et al. eds. General Thoracic Surgery, 7th edition. Philadelphia: Lippincott Williams & Wilkins, 2009:1387-425.
- Asamura H. Lymph node dissection for lung cancer. In: Shields TW, LoCicero J III, Reed CE, et al. eds. General Thoracic Surgery, 7th edition. Philadelphia: Lippincott Williams & Wilkins, 2009:1427-33.
- Watanabe Y, Shimizu J, Oda M, et al. Improved survival in left non-small-cell N2 lung cancer after more extensive operative procedure. Thorac Cardiovasc Surg 1991;39:89-94. [PubMed]
- Hata E, Hayakawa K, Miyamoto H, et al. Rationale for extended lymphadenectomy for lung cancer. Theor Surg 1990;5:19-25.
- Gaer JA, Goldstraw P. Intraoperative assessment of nodal staging at thoracotomy for carcinoma of the bronchus. Eur J Cardiothorac Surg 1990;4:207-10. [PubMed]
- Takizawa T, Terashima M, Koike T, et al. Mediastinal lymph node metastasis in patients with clinical stage I peripheral non-small-cell lung cancer. J Thorac Cardiovasc Surg 1997;113:248-52. [PubMed]
- Riquet M, Manac’h D, Saab M, et al. Factors determining survival in resected N2 lung cancer. Eur J Cardiothorac Surg 1995;9:300-4. [PubMed]
- Izbicki JR, Thetter O, Habekost M, et al. Radical systematic mediastinal lymphadenectomy in non-small cell lung cancer: a randomized controlled trial. Br J Surg 1994;81:229-35. [PubMed]
- Deslauriers J, Grégoire J. Clinical and surgical staging of non-small cell lung cancer. Chest 2000;117:96S-103S. [PubMed]
- Wong SL, Ji H, Hollenbeck BK, et al. Hospital lymph node examination rates and survival after resection for colon cancer. JAMA 2007;298:2149-54. [PubMed]
- Compton CC. Optimal pathologic staging: defining stage II disease. Clin Cancer Res 2007;13:6862s-70s. [PubMed]
- Berger AC, Sigurdson ER, LeVoyer T, et al. Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol 2005;23:8706-12. [PubMed]
- Benson AB 3rd, Schrag D, Somerfield MR, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol 2004;22:3408-19. [PubMed]
- Doddoli C, Aragon A, Barlesi F, et al. Does the extent of lymph node dissection influence outcome in patients with stage I non-small-cell lung cancer? Eur J Cardiothorac Surg 2005;27:680-5. [PubMed]
- Wu YC, Lin CF, Hsu WH, et al. Long-term results of pathological stage I non-small cell lung cancer: validation of using the number of totally removed lymph nodes as a staging control. Eur J Cardiothorac Surg 2003;24:994-1001. [PubMed]
- Lardinois D, De Leyn P, Van Schil P, et al. ESTS guidelines for intraoperative lymph node staging in non-small cell lung cancer. Eur J Cardiothorac Surg 2006;30:787-92. [PubMed]
- Tsang GM, Watson DC. The practice of cardiothoracic surgeons in the perioperative staging of non-small cell lung cancer. Thorax 1992;47:3-5. [PubMed]
- Little AG, Rusch VW, Bonner JA, et al. Patterns of surgical care of lung cancer patients. Ann Thorac Surg 2005;80:2051-6; discussion 2056. [PubMed]
- Boffa DJ, Allen MS, Grab JD, et al. Data from The Society of Thoracic Surgeons General Thoracic Surgery database: the surgical management of primary lung tumors. J Thorac Cardiovasc Surg 2008;135:247-54. [PubMed]
- Osarogiagbon RU, Yu X. Mediastinal lymph node examination and survival in resected early-stage non-small-cell lung cancer in the surveillance, epidemiology, and end results database. J Thorac Oncol 2012;7:1798-806. [PubMed]
- Verhagen AF, Schoenmakers MC, Barendregt W, et al. Completeness of lung cancer surgery: is mediastinal dissection common practice? Eur J Cardiothorac Surg 2012;41:834-8. [PubMed]
- Izbicki JR, Passlick B, Karg O, et al. Impact of radical systematic mediastinal lymphadenectomy on tumor staging in lung cancer. Ann Thorac Surg 1995;59:209-14. [PubMed]
- Bollen EC, van Duin CJ, Theunissen PH, et al. Mediastinal lymph node dissection in resected lung cancer: morbidity and accuracy of staging. Ann Thorac Surg 1993;55:961-6. [PubMed]
- Keller SM, Adak S, Wagner H, et al. Mediastinal lymph node dissection improves survival in patients with stages II and IIIa non-small cell lung cancer. Eastern Cooperative Oncology Group. Ann Thorac Surg 2000;70:358-65; discussion 365-6. [PubMed]
- Naruke T. Significance of lymph node metastases in lung cancer. Semin Thorac Cardiovasc Surg 1993;5:210-8. [PubMed]
- Yoshino I, Nakanishi R, Osaki T, et al. Unfavorable prognosis of patients with stage II non-small cell lung cancer associated with macroscopic nodal metastases. Chest 1999;116:144-9. [PubMed]
- Romero L. Influence of the mediastinal lymphadenectomy in non small cell lung cancer prognosis. Doctoral Thesis. 2007. Available online: http://hdl.handle.net/10803/4307
- Wu YI, Huang ZF, Wang SY, et al. A randomized trial of systematic nodal dissection in resectable non-small cell lung cancer. Lung Cancer 2002;36:1-6. [PubMed]
- Lardinois D, Suter H, Hakki H, et al. Morbidity, survival, and site of recurrence after mediastinal lymph-node dissection versus systematic sampling after complete resection for non-small cell lung cancer. Ann Thorac Surg 2005;80:268-74; discussion 274-5. [PubMed]
- Sakurai H, Asamura H, Watanabe S, et al. Clinicopathologic features of peripheral squamous cell carcinoma of the lung. Ann Thorac Surg 2004;78:222-7. [PubMed]
- Manser R, Wright G, Hart D, et al. Surgery for early stage non-small cell lung cancer. Cochrane Database Syst Rev 2005;CD004699. [PubMed]
- Gajra A, Newman N, Gamble GP, et al. Effect of number of lymph nodes sampled on outcome in patients with stage I non-small-cell lung cancer. J Clin Oncol 2003;21:1029-34. [PubMed]
- Ou SH, Zell JA. Prognostic significance of the number of lymph nodes removed at lobectomy in stage IA non-small cell lung cancer. J Thorac Oncol 2008;3:880-6. [PubMed]
- Xu F, Qi L, Yue D, et al. The effect of the extent of lymph node dissection for stage IA non-small-cell lung cancer on patient disease-free survival. Clin Lung Cancer 2013;14:181-7. [PubMed]
- Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg 2011;141:662-70. [PubMed]


