Gavin M. Wright: current treatments for NSCLC
Dr. Gavin M. Wright (Figure 1) is Clinical Associate Professor of University of Melbourne; Executive Member in Division of Surgery, St Vincent’s Hospital; and Management Advisory Committee of Western & Central Metropolitan Integrated Cancer Service. He is also Fellow of Royal Australasian College of Surgeons (RACS).
TLCR: In recent years, genotype-based molecular targeted therapy has been the breakthrough of advanced non-small cell lung cancer therapy. Could you please share with us your new findings in molecular targeted therapy for lung cancer?
Dr. Wright: Targeting the EGFR mutation with gefitinib or erlotinib has become the mainstream. But these gene alterations affect only a small proportion of all lung cancer patients. So we do need to find other molecular targets. The ALK fusion is also being well treated by crizotinib. We now have some new targets in squamous cell lung cancer. My collaboration found FGFR1 amplification that we reported few years ago.
More recently, we reported a new recurring fusion (NRG1-CD74), which appears in non-smoking patients with a particular type of non-small cell lung cancer—invasive mucinous adenocarcinoma. It should be treatable with trastuzumab, which is normally used in HER2 positive breast cancer.
There are obviously many targets that are represented in small numbers of lung cancers being reported—for example BRAF mutation being successfully treated with dabrafenib or vemurafenib. And we expect there will be an increase of the number of targets we can treat. I think eventually we probably have to move toward some sort of multiplex genomic testing to give everyone a chance to determine their own cancer targets.
TLCR: What is the significance of oligometastases in non-small cell lung cancer therapy? What are the essentials for treating these patients?
Dr. Wright: We find that there seems to be special cases in oligometastatic lung cancer where there is limited brain metastasis and a controllable primary lung cancer. In my institution, we aggressively treat such patients. We treat the lung cancer with surgery or sometimes radiotherapy, resect the brain metastasis, give whole brain radiation therapy and also adjuvant chemotherapy. That particular group seems to do much better that all other metastatic lung cancer with long-term survival.
Now that we have the molecular therapy, obviously we would resect these patients as well and given that brain is one place where the targeted therapy with EGFR tyrosine kinase inhibitors can be less effective, it is important to treat them with surgery and brain radiation.
TLCR: Video-assisted thoracic surgery (VATS) is becoming more and more important for thoracic tumors. Could you please explain the roles of VATS as a minimally invasive treatment for non-small cell lung cancer?
Dr. Wright: VATS has been applied for quite a long time. In fact, VATS lobectomies have now been done for over 20 years. However, it has been very slow to be taken up around the world, particularly in some countries. Even in quite advanced countries, it is still very slow to take up.
When we started doing VATS, it was just the occasional case that was ideal. In those cases the patients had a very small tumor, they are peripheral tumors, they have a perfect fissure, etc. It was offered only to a very small percentage of patients. Then we gradually developed the technique to the point that only rare patients would get open thoracotomy that have a very large tumor, or in very complicated situations. Almost all cases and even quite complex operations can now be performed with the VATS technique. For example, the patient in Figure 2 had a very proximal lung cancer originating in the right upper lobe but extending into the main right bronchus (airway). A simple lobectomy was not possible, and a pneumonectomy (removal of the whole lung) would involve removal of two lobes of healthy tissue. I decided to perform a right upper lobectomy by VATS with en bloc, or contiguous removal of the affected part of the main bronchus as a margin.
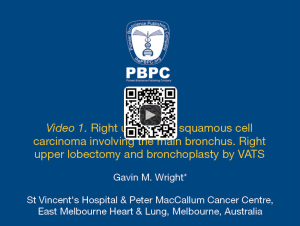
Following are the steps:
- The right upper lobe tributary of the superior pulmonary vein has already been divided;
- The pulmonary artery branches to the right upper lobe are divided with a stapler (truncus branch) and a ligature (recurrent branch);
- Fissure between the upper and middle lobes is created with a stapler;
- Bronchus cut open to expose the tumour and separate the lobe;
- Lobe is removed in a specimen bag;
- Extra margin is cut from the main bronchus;
- Airway reconstructed with running suture.
The patient went home on day 5 and is now very well. The tissue margins around the tumor were clear and no lymph nodes were involved. The patient did not require any further treatment.
TLCR: What do you think of the current clinical treatment and basic research of lung cancer in China? Are there any aspects still to be improved?
Dr. Wright: I think there are two aspects.One is that, obviously, China and places like Japan have differences in the range of patients (in terms of mutations) from western countries where we are used to investigating. For example, in Australia, considerably less than a third of adenocarcinomas would have an EGFR mutation, whereas in Eastern Asia, these make up perhaps up to a half or more of all cases. In one way, this is an advantage for China. However, patients do acquire resistance to EGFR inhibitors. I think the focus of research in China should probably be on resistance mechanisms. Because you have already have a good treatment for many patients, but the later failure of those treatments is what needs to be studied. As China has the population, the ability to get sufficient numbers of different resistance mechanisms, it is ideal for developing clinical trials here or elsewhere. I think China is a very fundamentally important place for that research.
TLCR: It is the first Sino-Australian Conference in Thoracic Oncology. Could you please share with us your prospect of cooperation and communication with China?
Dr. Wright: I think from the communication perspective, there are very great opportunities for collaboration. The barrier is usually with regulatory authorities, which unfortunately tend to block constructive interaction. You can see from this conference how much interaction there is between Australian and Chinese colleagues, and that is very fruitful at the individual level. But to get large-scale cooperation, it really requires the action of government and regulatory bodies, and we have less influence in those fields.
TLCR: Thank you very much!
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Wang MJ. Right upper lobe squamous cell carcinoma involving the main bronchus. Right upper lobectomy and bronchoplasty by VATS. Asvide 2014;1:263. Available online: http://www.asvide.com/articles/276
(Science Editor: Molly J. Wang, TLCR, editor@tlcr.org)