
Transesophageal needle aspiration using a third-generation Olympus ultrasound bronchoscope for subaortic lesions: a report of two cases
Introduction
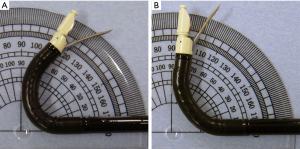
Transesophageal endoscopic ultrasound with bronchoscope-guided fine needle aspiration (EUS-B-FNA) using an endobronchial ultrasound (EBUS) bronchoscope has been reported to be useful for diagnosing mediastinal lesions (1) and for mediastinal staging of lung cancer in combination with endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) (2,3). In 2018, a third-generation Olympus EBUS bronchoscope (BF-UC290F; Olympus, Tokyo, Japan, Figure 1A) was launched. It has a 40° wider up-angulation range of the bending section and a 5° steeper needle angle compared to a conventional second-generation EBUS bronchoscope (BF-UC260FW; Olympus; Figure 1B). The new EBUS bronchoscope is preferable for evaluating previously difficult-to-reach lesions by EUS-B-FNA, including subaortic lesions. Here, we present two cases in accordance with the CARE-Guidelines (4).
Case presentation
Case 1
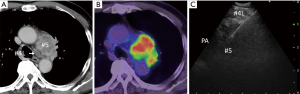
A 70-year-old woman was referred to our hospital to determine the cause of left recurrent nerve paralysis. She complained of hoarseness to the referring otolaryngologist and had been given a diagnosis of left recurrent nerve paralysis. She was a never-smoker with no medical history. In our hospital, a chest X-ray and computed tomography were taken, and revealed a tumor in the left upper lobe lung and an enlarged subaortic lymph node measuring 25 mm in shortest diameter (Figure 2A).

After informed consent was obtained, EUS-B-FNA through the esophagus was performed under local anesthesia and conscious sedation in the supine position for staging and diagnostic purposes. First, a conventional EBUS bronchoscope (BF-UC260FW; Figure 1B) was advanced through the esophagus, and the subaortic lymph node was observed endosonographically. We tried to perform a needle puncture using a 19-gauge needle (ViziShot 2 Flex; Olympus); however, the needle only reached the left lower paratracheal lymph node and not the subaortic lymph node (Figures 2,3). The result of rapid on-site cytological evaluation (ROSE) using a quick staining method (Diff-Quik; Kokusaishiyaku; Kobe, Japan) was negative. Then, we changed the conventional EBUS bronchoscope to the new EBUS bronchoscope (BF-UC290F; Figure 1A) and attempted a needle puncture in the subaortic lymph node. The needle reached the subaortic lymph node easily (Figures 2C,3), and the result of ROSE was positive after the first puncture. A total of four passes were performed to obtain an adequate quantity of histological material. There were no complications. She was given a final diagnosis of adenocarcinoma according to immunohistochemical staining of histological specimens obtained from the subaortic lymph node by EUS-B-FNA.
Case 2
A 63-year-old man with no symptoms and no relevant medical history, but who was a current smoker, underwent a medical examination; the chest X-ray revealed an enlarged mediastinum. Chest computed tomography revealed a subaortic lesion 38 mm in the shortest diameter (Figure 4A); this was hypermetabolic on positron emission tomography-computed tomography (Figure 4B). EBUS-TBNA was performed using a conventional EBUS bronchoscope (BF-UC260FW), but the result was non-diagnostic; the patient was referred to our hospital for examination of the subaortic lesion. After obtaining written informed consent, EUS-B-FNA was performed using the new EBUS bronchoscope (BF-UC290F) and a 19-gauge needle, as described above for Case 1 (Figure 4C). ROSE was positive at the third puncture and a total of five passes were performed. There were no complications. Immunohistochemical staining of the histological specimens obtained via EUS-B-FNA was suggestive of metastatic adenocarcinoma.
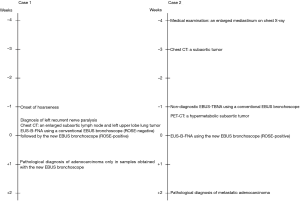
The timelines of Cases 1 and 2 are shown in Figure 5.
Discussion
The combination of EBUS-TBNA and endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) is recommended for mediastinal staging of lung cancer, and EUS-B-FNA is considered an alternative to conventional EUS-FNA (2,3). The reported diagnostic utility of EUS-B-FNA is comparable to that of conventional EUS-FNA (3); however, conventional EUS-FNA has an advantage of superior ability to access subaortic lesions. The dedicated EUS endoscope has strong bending power that is not easily affected by needle stiffness, a wide bending angulation range (130°–150° up-angulation), and a needle elevator that can be used to adjust the needle puncture angle. On the other hand, the bending power of the previous EBUS bronchoscope is insufficient for flexing the bronchoscope when a stiff needle is used; the bending capability is only 120° up-angulation, and the protruding needle angle is nonadjustable and gentle. Thus, several investigators have reported good accessibility of EUS-FNA using a dedicated EUS endoscope for subaortic lymph nodes (6), while only a few cases of successful evaluation of subaortic lymph nodes by EUS-B-FNA have been reported (7,8).
Since the first generation of EBUS bronchoscopes was launched in 2004, EBUS bronchoscopes and dedicated EBUS needles have improved, enabling better access to mediastinal regions through the airway and esophagus. The new EBUS bronchoscope has an up-angulation range of 160°, and the protruding needle angle is 5° steeper than that of previous EBUS bronchoscopes. In addition, the 19-gauge EBUS needle used in these cases was more flexible than the thinner 21- and 22-gauge EBUS needles. Although still technically challenging, the combined use of a new EBUS bronchoscope and a flexible EBUS needle may provide greater opportunity to evaluate subaortic lesions.
Limitations
This study was performed using only two cases; further large-scale studies are necessary to elucidate the usefulness of EUS-B-FNA with the new EBUS bronchoscope for evaluating subaortic lesions.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved. Informed consent for publication was obtained in writing from Cases 1 and 2.
References
- Oki M, Saka H, Ando M, et al. Transbronchial vs transesophageal needle aspiration using an ultrasound bronchoscope for the diagnosis of mediastinal lesions: a randomized study. Chest 2015;147:1259-66. [Crossref] [PubMed]
- Vilmann P, Clementsen PF, Colella S, et al. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Endoscopy 2015;47:545-59. [Crossref] [PubMed]
- Korevaar DA, Crombag LM, Cohen JF, et al. Added value of combined endobronchial and oesophageal endosonography for mediastinal nodal staging in lung cancer: a systematic review and meta-analysis. Lancet Respir Med 2016;4:960-8. [Crossref] [PubMed]
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Oki M, Saka H, Kogure Y. An ultrasound video of the evaluation of a case of lung adenocarcinoma with subaortic lymphadenopathy that could not be diagnosed via EUS-B-FNA using a conventional ultrasound bronchoscope, but that was successfully evaluated and diagnosed employing a new ultrasound bronchoscope. Asvide 2019;6:355. Available online: http://www.asvide.com/watch/33040
- Liberman M, Sampalis J, Duranceau A, et al. Endosonographic mediastinal lymph node staging of lung cancer. Chest 2014;146:389-97. [Crossref] [PubMed]
- Hwangbo B, Lee GK, Lee HS, et al. Transbronchial and transesophageal fine needle aspiration using an ultrasound bronchoscope in mediastinal staging of potentially operable lung cancer. Chest 2010;138:795-802. [Crossref] [PubMed]
- Oki M, Saka H, Ando M, et al. Endoscopic ultrasound-guided fine needle aspiration and endobronchial ultrasound-guided transbronchial needle aspiration: Are two better than one in mediastinal staging of non-small cell lung cancer? J Thorac Cardiovasc Surg 2014;148:1169-77. [Crossref] [PubMed]


