A 61-year-old man with cough and white sputum
A 61-year-old man was admitted to this hospital because of cough and white sputum on March 16, 2011.
History of disease
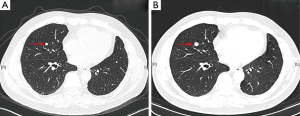
The patient had been in his usual state of health until approximately two months before admission, on early January of 2011, when paroxysms of coughing and white sputum appeared. The patient paid no attention to the symptoms and had no special treatment. The symptoms of cough and sputum kept continued for the next two months and had no release. On March 15, the patient visited the respiratory clinic in the first hospital and took a computed tomography (CT) scanning of his lung. There was an abnormal pulmonary mass in the left lower lobe in the CT imaging (Figure 1), so the patients was admitted to our hospital for the diagnosis and further treatment. The patient had neither particular previous medical history nor smoking history.

Body examination
On examination, the temperature, the blood pressure, the pulse, the respiratory rate and the oxygen saturation were all in the normal range. There was no enlarged superficial lymph node. The examination of respiratory system and the rest body organs was normal.
Laboratory data
There was no abnormal index in blood routine examination, blood biochemistry and tumor markers such as carcinoembryonic antigen (CEA), CYFRA 21-1, neuron specific enolase (NSE) and SCC.
ECG and pulmonary function test were normal. Follow-up positron emission tomography/CT (PET/CT) scanning of whole body reported that the size of pulmonary mass was 3.0 cm × 2.2 cm, 18F-FDG uptake was increased in this mass with a maximum standardized uptake value (SUVmax) of 6.6 and there was no evidence of metastasis in other organs and lymph nodes. MRI imaging of brain was normal.
First diagnosis
The lung cancer multidisciplinary team (MDT) discussed the condition of the patient.
Respiratory physician: a 61-year-old male patient, with paroxysmal cough and white sputum lasting for more than two months and had no release. CT scanning reported an abnormal mass in the left lower lung lobe with an increased SUVmax uptake value shown in PET/CT. All these evidence suggested a large probability of lung cancer. If there was no contraindication, surgical resection could play an important role in both diagnosis and treatment.
Cardiothoracic surgeon: this patient had no particular previous history, lung function was normal, performance status (PS) score was 0, and the lesion was single with no lymph node and distal metastasis. Taken these together, there was no contraindication for the surgery.
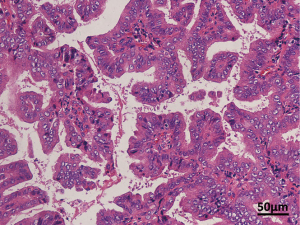
The patient took the left lower lobe resection and lymphadenectomy on March 22, 2011. The histological pathology of the lesion, hilar lymph node and “7 group” lymph node suggested adenocarcinoma (Figure 2). The patient was finally diagnosed as left lung adenocarcinoma with TNM stage IIIA (pT3N2M0), and no EGFR mutation according to the ARMS sequence technology.

Treatment and follow-up
How to treat and follow-up
Respiratory physician: according to the NCCN guideline, the patient took four cycles of postoperative chemotherapy with pemetrexed 0.8 g and nedaplatin 120 mg during April to June in 2011, following with three month a time chest CT scanning.
Another nodule appeared
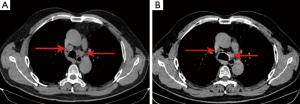
The disease kept stable until April 11, 2012. There was a solitary pulmonary nodule (SPN) with a max diameter of 5.5 mm appeared in the middle lobe of right lung in CT scanning. Followed up to June 27, this nodule grew larger (Figure 3). The whole body examination found no other metastasis.
Second diagnosis and treatment
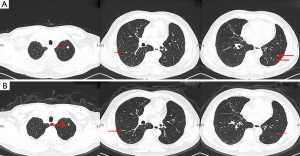
Again, the lung cancer MDT discussed the condition: respiratory physician took the idea that since the patient was histologically diagnosed as adenocarcinoma in the left lung at TNM stage of IIIA, the SPN in right lung would be thought as metastasis. However, there is no evidence of other metastasis and this single lesion could be resected to be diagnosed histologically. Cardiothoracic surgeon evaluated the patient that there was no contraindication for the surgery. The patient took a second operation “the right middle lobe resection” on July 03, 2011. The histological pathology of the lesion again suggested adenocarcinoma and there were no lymph node metastasis (Figure 4). The patient was diagnosed as left lung adenocarcinoma at TNM stage IV (pT3N2M1a, two lungs) with neither EGFR mutation nor ALK-EML4 fusion gene.
Respiratory physician: according to the new stage, the patient took another four cycles of postoperative chemotherapy with docetaxel 120 mg and nedaplatin 120 mg during July to October in 2012, following with three months a time chest CT scanning.
Disease development
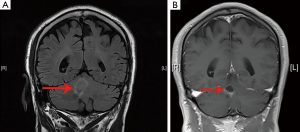
In the middle April of 2013, cough and white sputum again appeared, together with hoarseness. The patient hospitalized and took another PET/CT scanning of whole body, which reported that several enlarged mediastinal lymph nodes, a SPN in left upper lobe and lesion in cerebellum had increased 18F-FDG uptake. The brain metastasis was also proved in brain MRI scanning.
Diagnosis and treatment
The lung cancer MDT discussed the condition for the third time.
Respiratory physician: the patient was now diagnosed as left lung adenocarcinoma at TNM stage IV (pT3N2M1b, brain) with neither EGFR mutation nor ALK-EML4 fusion gene and had a progressive disease. The followed whole body therapy should be used and the local treatment in advanced NSCLC patient should also be applied. In the third-line therapy, the patient may try to take the EGFR-TKI as a targeted therapy, although the EGFR mutation was null.
Radiation therapist: enlarged mediastinal lymph nodes could be the reason for hoarseness. According to the NCCN guideline, radiation therapy should be taken to both lymph nodes and the brain metastasis.
From June 17 to June 20, the patient took the stereotactic radiotherapy for metastatic mediastinal lymph nodes with DT: 40 Gy/4 fx, average dosage 80%. Chest CT showed the mediastinal lymph nodes were significantly reduced on July 25, 2013 (Figure 5).
The patients took erlotinib 150 mg once a day after the stereotactic radiotherapy. However, the number of small lesions on lungs was increased and the brain metastasis was enlarged on October 22, 2013. The lung cancer MDT discussed the condition for the fourth time: respiratory physician diagnosed the patient had a progressive disease, which indicated that the targeted therapy was ineffective. Since the brain metastasis developed, radiation therapist thought radiation therapy must be taken on the brain metastasis.
The stereotactic radiotherapy for the single brain metastasis was taken four days since October 30, 2013. Since October 2013, patient had single agent chemotherapy of abraxane 400 mg. The whole body examination suggested that there was progression-free after two cycles of chemo. Chest CT scanning reported the small nodes on lung were decreased (Figure 6) and brain metastasis was also smaller on the MRI image (Figure 7).
Follow-up
The patient is now diagnosis as left lung adenocarcinoma, TNM stage IV (pT3N2M1b, brain), took five cycles of single agent chemotherapy of abraxane. The latest whole body examination showed disease was stable with no new lesions and metastasis, PS score is 0 and the overall survival (OS) time is 34 months.
Key points for discussion
- During the process of diagnosis and treatment in the patient, lung cancer MDT took four times discussions on the condition of the patient and proposed the most suitable solution. The OS of the patient who is without EGFR mutation is predicted to be more than three years, which reflects the success of MDT in the treatment. Since the multidisciplinary treatment is the most promising development of the lung cancer diagnosis and treatment, what are the future and further improvement and the suggestion in lung cancer MDT?
- According to the ARMS seq, the EGFR mutation was null in this patient and the response of the targeted therapy also proved that the EGFR-TKI use has rare effect. Should the status of EGFR mutation be the definite criterion of the EGFR-TKI use or the patient could try EGFR-TKI in a multi-line therapy although there is no mutation or the mutation status is unknown?
- After the resection of primary lesion in the left lung and postoperative chemotherapy, the patients took another resection of the new SPN appeared in right lung which was thought to be a metastatic lesion. The second resection is one feature of the case and maybe the reason for the OS time of 34 months in advanced NSCLC patient. What is the possibility and suggestion about the operation in metastatic NSCLC patient?
- When the patient developed into stage IV as advanced NSCLC, not only the systemic therapy such as chemotherapy and targeted therapy, but also the local treatment like stereotactic radiotherapy for metastatic mediastinal lymph nodes and brain metastasis were applied in him, and the response was considerable. Is the local treatment necessary in the advanced lung cancer patient when the whole body treatment is also applied? What is the best time to apply the local treatment to advanced patient? What is the suggestion and experience for the local treatment?
Acknowledgements
Disclosure: The authors declare no conflict of interest.


