Analysis of lung adenocarcinoma with bone metastasis: a case report
Introduction
Recently, accumulating studies have focused on the drug research of advanced lung cancer. Treatment strategies from the traditional platinum-containing dual-drug chemotherapy mode to targeted therapy, anti-angiogenic drugs (1), immunotherapy and other single-agent or combination drugs, bring larger survival benefits for patients with advanced lung cancer. Non-small cell lung cancer, especially lung adenocarcinoma, is often associated with positive oncogenes overexpression and the TKI drug monotherapy model for patients of advanced lung cancer with epidermal growth factor receptor (EGFR) gene mutations was set up. AURA3 studies showed that patients with T790M mutation after the first-generation TKI resistance were treated with osimertinib can still achieve better survival benefits (2). FLAURA study further showed that first-line treatment with osimertinib resulted in the longest PFS of 18.9 months. However, lung cancer patients, especially those with lung adenocarcinoma, often have single or multiple bone metastases at the time of diagnosis or drug treatment (3). Lung cancer with bone metastases, especially metastases in weight-bearing joints such as spinal bone, often causes untold suffering, including pain, nerve compression-induced physical activity disorders, and disability (4). Currently, the treatment options for bone metastasis are pain relief, bone metabolism improvement, local radiotherapy, and radionuclide therapy. Conventional medical treatments including chemotherapy, targeted therapy, anti-angiogenic drugs, and immunotherapy are not found obvious advantages in bone metastases of lung cancer. In this case, patient with advanced lung adenocarcinoma and EGFR gene mutation was resistant to gefitinib, and then T790M was detected, and the primary disease was controlled after treatment with osimertinib. Nevertheless, despite the use of analgesia, bone metabolism improvement therapy and local radiotherapy, the adverse consequences of bone metastasis still had not avoided. We believe that the treatment goal of patients with advanced lung cancer is to extend the survival of patients with high quality. Reporting this case is to suggest that the researchers should make further efforts in the systematic treatment and palliative treatment of bone metastasis of lung cancer, to obtain better quality of life for patients.
Case presentation
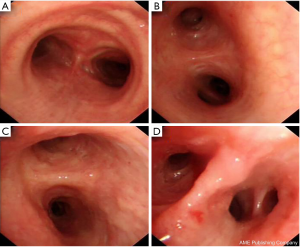
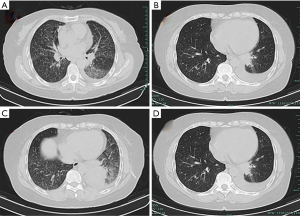
A 65-year-old woman was admitted to our hospital, she had a cough, expectoration, chest distress, and shortness of breath for half a month. The left breath sounds were low, and a few moist rales were found in the left lung. Pulmonary CT from other hospitals shows space-occupying lesions but without detailed analysis. Hence, a PET/CT examination was carried out, and we found that: there was soft tissue mass in the basal segment of the inferior lobe of the left lung, which was of the high possibility of central lung cancer. The patient was with obstructive pneumonia and with diffuse solid nodules in the two lungs, interlobar pleura and mediastinal pleura, which was considered as hematogenous metastasis. Moreover, the left hilar lymph node was enlarged, considering as lymphatic metastasis. The left 6/8 rib, the right iliac crest, the 7th cervical vertebra, the 4th lumbar inferior articular process, and the first sacral vertebra were damaged. Therefore, multiple bone metastasis and left pleural effusion were considered. On 2018-10-11, in the Fourth Hospital of Zhejiang Medical University, examination showed that carcinoembryonic antigen was 8.79 ng/mL, erythrocyte sedimentation rate, anti-nuclear antibody, T-spot were negative. On admission, closed chest drainage guided by B-ultrasound was conducted, and exfoliated cells in hydrothorax were examined, enhanced CT of the lungs, percutaneous pulmonary puncture, and bronchoscopy under CT guidance were improved. Results: (I) pulmonary enhanced CT: there was mass in the left lower lobe, considering central lung cancer and obstructive pneumonia, multiple nodules in both lungs, sub-pleural area, interlobar pleura, and mediastinum. Enlarged lymph nodes were found in hilar and mediastinum. Local bone destruction in the left sixth and eighth rib was detected, which was considered as multiple metastases. Meanwhile, the patient was with left pleural effusion with left lower lobe expansion and insufficiency (Figure 1). (II) Decapitation cells from pleural effusion: on November 11, 2018, cancer cells were found in left pleural effusion fluid-based cytology examination and was considered as adenocarcinoma. (III) Adenocarcinoma infiltration in the mucosa was found by bronchoscopy biopsy and trachea biopsy in the middle lobe of the right lung (Figure 2). (IV) Adenocarcinoma was considered by percutaneous lung biopsy. Diagnosis: lung adenocarcinoma with T4N3M1 in stage IV. Targeted gene detection in percutaneous lung puncture suggested EGFR 21 L858R positive, and the patient was treated with gefitinib (250 mg, p.o, q.d) combined with tramadol. Admission evaluation on 2019-2-22: pulmonary CT: mass was similar to the past, pleural effusion was reduced, CEA was 2.09 ng/mL, B-ultrasound in the superficial lymph node, liver, pancreas, spleen, kidney, adrenal gland and thyroid were normal, head CT was normal. Admission assessment on 2019-5-9: pain in bone was more obvious than before, pulmonary CT: small nodules in both lungs were more than before, CEA concentration was 5.79 ng/mL, B-ultrasound of superficial lymph nodes, liver, pancreas, spleen, kidney, adrenal gland, and thyroid gland were normal. The head CT was normal. T790M was positive in blood, osimertinib (80 mg p.o, q.d) + tramadol + zoledronic acid was administrated for symptomatic treatment. The head CT is normal. On 2019-7-26, PET/CT results showed: (I) soft tissue density shadow in the posterior basal segment of the lower lobe of the left lung near the hilum, FDG metabolism slightly increased, considering that tumor activity was inhibited after targeted therapy; (II) multiple mildly enlarged lymph nodes were found in bilateral hilum and mediastinum (zone 4R and zone 7), partial FDG metabolism was detected, considering reactive hyperplasia of lymph nodes; (III) the right iliac crest, sacrum, the 7th vertebra of the neck, the 2nd spinous process of the thoracic, the 4th vertebra of the lumbar and its accessories, the 3rd and 4th rib of the right side and the 8th rib of the left side were damaged locally, and FDG metabolism was increased. Therefore, multiple bone metastases were considered; (IV) multiple small nodules were seen in both lungs and sub-pleura. No obvious abnormalities were observed in FDG metabolism; hence, inflammatory nodules were considered; (V) local bone density was increased in the 6th rib on the left, FDG metabolism showed no obvious abnormalities, close follow-up was recommended; (VI) left pleural effusion was present. At present, this patient has poor control of bone metastasis, and no obvious improvement is seen after zoledronic acid treatment. The pain is still severe after two courses of local radiotherapy in the lumbar spine, and the right limb movement was not good after resection. Systemic nuclide therapy is recommended.
Discussion
The patient was initially diagnosed with lung adenocarcinoma with bone metastasis, and the pathological examination revealed it to be EGFR-positive. After treatment with TKI gefitinib, the tumor was stable. After follow-up, drug resistance occurred. The blood samples had shown a positive result of T790M. After the treatment of TKI osimertinib, primary tumor control therapy was followed, but the patient's bone metastasis was poorly effective.
Furthermore, the patient status did not improve after treatment of pain relief, bone metabolism improvement and local radiotherapy in weight-bearing bone, and the physical activity were unfavorable. Admittedly, TKI treatment is the first choice for lung adenocarcinoma with EGFR positive (5), and studies have shown that TKI can also be combined with chemotherapy or anti-angiogenic drugs. However, the earlier study did not conduct a subgroup analysis of bone metastases, and there was no systematic treatment plan for bone metastases so far. This patient still had poor control of bone metastases despite effective primary tumor control, which markedly affects the survival treatment. This case reminds us that higher life quality is equally important to long-term survival; more researches are needed on systemic and local treatment of bone metastasis of lung cancer.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 2006;355:2542-50. [Crossref] [PubMed]
- Akamatsu H, Katakami N, Okamoto I, et al. Osimertinib in Japanese patients with EGFR T790M mutation-positive advanced non-small-cell lung cancer: AURA3 trial. Cancer Sci 2018;109:1930-8. [Crossref] [PubMed]
- Li S, Peng Y, Weinhandl ED, et al. Estimated number of prevalent cases of metastatic bone disease in the US adult population. Clin Epidemiol 2012;4:87-93. [PubMed]
- Dunne EM, Fraser IM, Liu M. Stereotactic body radiation therapy for lung, spine and oligometastatic disease: current evidence and future directions. Ann Transl Med 2018;6:283. [Crossref] [PubMed]
- Asami K, Okuma T, Hirashima T, et al. Continued treatment with gefitinib beyond progressive disease benefits patients with activating EGFR mutations. Lung Cancer 2013;79:276-82. [Crossref] [PubMed]