‘One-stop shop’: lung cancer patients’ and caregivers’ perceptions of multidisciplinary care in a community healthcare setting
Introduction
Lung cancer accounts for 27% of all US cancer-related deaths. The 5-year survival of all patients diagnosed annually has only increased from 12% to 17% over the past 4 decades (1). These dismal statistics reflect disease biology, but also the inherent difficulty of caring for patients with lung cancer, who are often enfeebled by cumulative age- and tobacco-related co-morbidities (2,3). In addition, care delivery is complicated because diagnosis, staging, and treatment require the involvement of multiple physicians with widely different skillsets, any of which may or may not be appropriate for individual patients (4).
The prevailing standard of care for lung cancer involves serial determination of patient needs by sequential referrals to specific care providers, including interventional radiologists, pulmonologists, thoracic surgeons, medical and radiation oncologists, and palliative care specialists. This serial care model, if not carefully coordinated, can introduce significant delays in care, and potential mismatches between patient needs and provider skill-sets (5-7). Theoretically, the multidisciplinary care model can mitigate this risk, and has been almost universally recommended as a means of improving the quality of care for cancer (4,5,8,9). However, the value of this model of care delivery has not been clearly established (10-12).
As a preliminary step towards a comparative effectiveness evaluation of serial and multidisciplinary care, we sought to understand patients’ perceptions of both models. Specifically, we attempted to elucidate patients’ and their caregivers’ experience of care within the two models, perceptions of barriers to implementing multidisciplinary care, and meaningful benchmarks with which to measure the quality of lung cancer care delivery.
Methods
With the approval of the Institutional Review Boards of the Baptist Cancer Center and the University of Memphis, both in Memphis, Tennessee, USA, we conducted focus groups of patients undergoing care for lung cancer, and their informal caregivers.
The Multidisciplinary Thoracic Oncology Program
The Multidisciplinary Thoracic Oncology Program consisted of a weekly half day clinic during which patients were concurrently seen by a thoracic surgeon, medical oncologist, and pulmonologist, with real-time radiology support and coordination by a nurse navigator. All patients were also discussed in a weekly conference involving a larger group of medical and radiation oncologists, pulmonologists, thoracic surgeons, pathologists, radiologists, and palliative care specialists (13). Recommendations were recorded and communicated back to clinicians responsible for actual care, irrespective of their level of participation in the program.
Patient-caregiver dyads
Patients who had received care related to an established or suspected lung cancer diagnosis within or out of the multidisciplinary thoracic oncology clinic in this community-based healthcare system in the preceding 6 months were invited to participate. Patients identified their specific informal caregiver, to form a patient-caregiver dyad.
Data collection
We conducted ten focus groups between March 2013 and January 2014. Patients and caregivers were separated in two different rooms to participate in the focus groups. A moderator and a note-taker introduced the study, obtained informed consent, conducted, audiotaped, and took notes on the focus group discussions. Each session was moderated by a Medical Anthropologist or Clinical Psychologist unaffiliated with the healthcare system. Participants were reassured of anonymity and confidentiality, in order to facilitate frank discussion. A standardized script was used to ensure consistency of questions across all focus groups. Each session lasted about 1-2 hours, resulting in over 15 hours of tapes and 256 pages of transcripts. Eight focus group sessions were conducted on the campus of the Baptist Memorial Hospital in Memphis. In order to provide the perspectives of patients from a rural environment distant from the location of the multidisciplinary clinic, we conducted two sessions in Grenada, Mississippi. The number of focus groups was not pre-specified, but rather was based on attainment of saturation in emerging themes.
Data analysis
We used verbatim transcripts of the audio recordings and field notes to analyze the content of each focus group session. Data were analyzed using Dedoose Software version 5.0.11, a web-based application for managing, analyzing, and presenting qualitative and mixed method research data (SocioCultural Research Consultants, LLC, Los Angeles, CA, USA). The software allows hierarchical linkage of codes for clear visualization of data structure. Three research team members independently reviewed these transcripts and developed a consensus plan to identify recurring themes and variants, using Dedoose. Collaborative coding, data reduction, display, and interpretation were conducted using Creswell’s 7-step analysis framework (14). Overlapping themes were given greater emphasis than non-overlapping themes. All initial codes and categories were sorted and compared until core categories of recurrent themes emerged as a basis for Grounded Theory (15).
Reliability and validity
We took steps to ensure rigor in the qualitative data collection and analysis. ‘Credibility’ (internal validity) was accomplished through member checking by asking participants in subsequent focus groups about topics mentioned during previous sessions; to increase ‘transferability’ (external validity), verbatim transcripts were used during data analysis to truly reflect the life-experiences of participants in their own words; ‘dependability’ (reliability) was enhanced by continual audits of transcripts against field notes and by research team members developing a consensus plan to ensure consistency throughout the data analysis process; finally, ‘confirmability’ was accomplished by using participants’ own words to support each theme, with multiple researchers considering the context and appropriateness (16,17).
Results
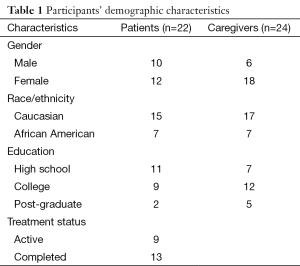
We conducted ten focus groups involving five patient-caregiver dyads, including 22 patients and 24 caregivers (one caregiver attended without a patient, and one patient attended with two caregivers). Patients had either completed treatment for lung cancer within 6 months or were actively undergoing therapy (Table 1). They covered the spectrum from early stage, with curative treatment intent, to advanced stage with palliative care. Several themes emerged from these qualitative analyses, which are summarized under subheadings, with illustrative quotations (Tables 2,3).
Full table
Full table
Full table
Perceptions of multidisciplinary care
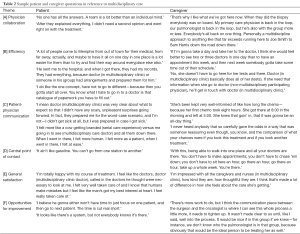
Physician collaboration
Participants preferred multiple specialists working together as a team to decide on the best plan of care. They believed that more input from different specialists decreased errors and confusion, resulting in a higher level of trust in the final treatment plan. Some felt that the multidisciplinary model provided a built-in second opinion (Theme [A] in Table 2).
Efficiency
Participants described how the amount of time dedicated towards travel, waiting for appointments, tests, and visits was reduced in the multidisciplinary care model. They preferred committing an entire day out of their schedule to see all the doctors to having their doctor visits stretched out over time. Participants reported how tests, such as CT, PET, or MRI scans, could be done efficiently and the results made available to all physicians. By coordinating these tests, they would not have to be repeated when a patient sees another specialist. Others described how the time dedicated towards cumbersome, repetitive paperwork may be reduced by only going to one location (Theme [B] in Table 2).
Patient-physician communication
Open and active patient-physician communication during the diagnosis and treatment process was deemed essential by many participants. This more active form of communication provided a sense of comfort. Patients and caregivers appreciated how they were always kept informed about succeeding steps and possible expectations so that they could better prepare for outcomes. The amount of one-on-one time spent between the patient and physician during an appointment was deemed to be vital. Patients and caregivers appreciated the sensitivity of the providers and how information was relayed in lay terms. This demonstrated the sincerity of the physicians and reassured the participants about prognosis, thus helping them to feel more at ease (Theme [C] in Table 2).
Central point of contact
Patients and caregivers preferred having a central point of contact to refer to for questions and scheduling appointments. They found it burdensome to have to seek care from multiple specialists. They preferred to have care decisions made at a central location rather than going from location to location, referring to the multidisciplinary clinic as a ‘one stop shop’. This was seen as very convenient. For many, it reduced anxiety and confusion associated with scheduling several appointments with multiple doctors and not knowing who to refer to for questions (Theme [D] in Table 2).
General satisfaction
Participants were generally satisfied with the level of care they received in the multidisciplinary clinic. Patients reported “feeling a lot better” or “feeling good” after treatment and appreciated the patient-centeredness of care (Theme [E] in Table 2).
Perceptions of serial care
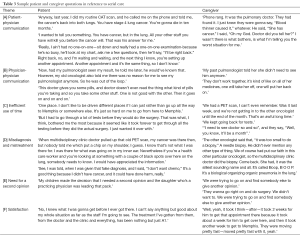
Patient-physician communication
The manner in which diagnosis and prognosis are communicated affected the care experience. Participants reported multiple incidents of insensitive disclosure of disease, such as when providers called patients on the telephone to inform them of the initial diagnosis of disease, rather than during a face-to-face office visit, which was deemed more appropriate. Some physicians seem too blunt and direct when explaining information to patients, which came across as insensitive or callous. Participants were largely dissatisfied with this style of communication. Some participants had difficulty gaining access to, and spending time with, their physicians. There were concerns about the lack of patient-physician dialogue due to lack of time. Some patients had difficulty discussing health concerns because physicians seemed hard to ‘pin down’ or never returned to the patient’s room during office visits (Theme [A] in Table 3).
Physician-physician communication
Some problems within the serial care model were due to the lack of doctor-to-doctor communication. This included failure to transfer medical records between healthcare establishments, to update patients’ other physicians on their status, and failure to collaborate to develop a care plan. Patients were concerned about avoidable complications occurring because of poor communication between their specialists. Participants expressed concerns about the lack of oversight of prescribed medications. Different doctors prescribe medications that counter-act each other or produce side-effects. Many felt that this process would continue until the communication between providers improves (Theme [B] in Table 3).
Inefficient use of time
Participants discussed the general inconvenience and time-cost of dealing with multiple physicians in different settings, multiple appointments, and numerous trips to offices. This was especially difficult for out-of-town patients. Being involved with multiple specialists also contributed to delays in diagnosis and treatment. Patients had to wait longer for follow-up appointments since they had to adhere to physicians’ schedules. Others experienced long delays, waiting for tests and results. This was unsettling to patients who were anxious to begin treatment (Theme [C] in Table 3).
Misdiagnosis/mistreatment
Some participants felt there was suboptimal evaluation when patients initially presented with symptoms, leading to under- or over-treatment, and even misdiagnosis. Conditions that could have been caught and treated early were not addressed by their physicians. Participants claim that they would appreciate such information, so that they could seek appropriate treatment in a timely manner. There were concerns that the lung cancer could have progressed during the time spent treating the wrong condition, or when the diagnosis was missed. Some patients reported being erroneously diagnosed with lung cancer and undergoing treatment, while some believed early tests that could have potentially revealed the lung cancer were ignored (Theme [D] in Table 3).
Need for second opinion
Participants generally desired a second opinion while under serial care, especially when patients were not comfortable with the initial diagnosis or treatment plan suggested. Many patients relied heavily on the opinions of their social support systems regarding second opinions, and were more likely to seek a second opinion if suggested by a caregiver or family member (Theme [E] in Table 3).
Satisfaction
Not all participants had a bad experience with serial care. Some participants were satisfied with the delivery of care provided through the serial care model. These participants reported having an open line of communication with providers, as well as a quick turnaround between appointments (Theme [F] in Table 3).
Opportunities for improving multidisciplinary care
Participants were encouraged to outline areas where the multidisciplinary clinic could improve.
Communication between doctors
Participants described room for improving communication between providers within the clinic, because of occasionally inconsistent messages relayed during the care process.
Amount of time spent with patients
Participants were also concerned about the possibility of limited one-on-one time between patients and physicians during office visits.
Clarity of model description and patient education about the model
Some participants were unaware that they were a part of the multidisciplinary clinic until later in the process. This information would have helped them better understand the logistics of the model, which was very different from their prior experience (Theme [F] in Table 2).
Benchmarks for model evaluation
To help us develop patient-centered benchmarks with which to measure the quality of implementation of the multidisciplinary care model, participants were asked to identify areas of highest priority to them. They identified clear, timely communication between physicians and patients/caregivers, consistency of physicians’ messages, adequate consultation time, timely physician-to-physician communication, timely care, and ease of access to care.
Patient-physician communication should ensure that patients and caregivers understand the diagnosis and treatment plan in lay terms; alternative options and the reasons for recommending specific options must be explained; members of the team should spend sufficient time with patients to keep them informed and answer their questions. The timeliness of care was another critical benchmark identified. The nurse navigator in the clinic was perceived as the key to alleviating problems with coordinating procedures, treatments, and appointments. Communication among physicians within and outside the multidisciplinary team was seen as pivotal in avoiding delays, conflicting messages, and redundant testing. To maximize benefit from the multidisciplinary care model, participants emphasized the need for easy access.
Discussion
Despite near-universal recommendation by experts (4,5,9,18), there is relatively little evidence to support the value of multidisciplinary care (10,12,19). Even the definition of ‘multidisciplinary care’ is highly variable, ranging from case discussions at tumor boards, to various formulations of group clinics at the other end of the spectrum (20). The practice is mostly limited to academic healthcare settings and other closed systems, such as the Veterans’ Affairs Healthcare System. However, >70% of lung cancer care in the US is delivered outside such environments.
In order to bridge the gap between expert recommendation and actual practice of multidisciplinary care, it is important to understand the value of multidisciplinary care (and answer the question, ‘why should it be done?’); expose the barriers to implementation (to answer the questions, ‘why is it infrequently done?’, and ‘can it be done?’); and to determine how best to measure the key attributes of effective multidisciplinary care in order to enable optimal implementation (to answer the question, ‘how should it be done?’), leading up to objective comparison to outcomes of standard serial care.
Prior reports have mostly covered provider perspectives on multidisciplinary care (21,22). However, care delivery systems exist to serve patients and caregivers. Patients depend on their caregivers for access to care, and caregivers share the emotional and financial burdens of sickness with patients (23,24). Their perspectives need to be considered carefully in any effort to develop effective and sustainable care-delivery programs.
The identified benefits of multidisciplinary care covered the Institute of Medicine’s six aims of healthcare quality improvement (patient-centeredness, safety, efficacy, efficiency, timeliness, and equity) (25). This by itself justifies the effort needed to develop multidisciplinary lung cancer care programs within community-based healthcare systems. For example, the belief that multidisciplinary care significantly improves the quality of communication about lung cancer, and patients’ level of trust in their proposed management, to the extent that second opinions were deemed unnecessary, is clearly a patient-centered benefit.
A single point of contact addresses the domains of efficiency and patient-centeredness. Less redundancy in testing, and fewer doctor visits suggests greater efficiency of care. Mapping out the pathway of care early and emphasizing same-day scheduling potentially improves the timeliness of care. It may also improve the appropriateness of pre-treatment testing and treatment selection, which may in turn improve the efficacy of treatment. Participants’ perceptions that the quality of care is better and the likelihood of mis-treatment is lower in the multidisciplinary care model, raise concerns about the safety and equity of care within the standard serial care model. Finally, access to more convenient and uniformly high quality care addresses the domain of equity.
In this qualitative study, we found that patients receiving care within a large, demographically and geographically diverse healthcare system, and their caregivers, strongly favor the multidisciplinary care model of lung cancer care delivery. Among other characteristics, the model was perceived to be more patient-centered and efficient. This suggests that establishing a multidisciplinary thoracic oncology program is likely to be favorably received by patients and their informal caregivers.
Limitations of this study include our qualitative, focus group-based approach which is subjective, relatively unstructured, and involves researchers’ interpretations of themes from transcripts of discussions. To provide objectivity to the analysis, we used the same script for all focus groups and had three researchers independently review the transcripts before developing consensus on recurrent themes. Our relatively small sample size may not fully represent all lung cancer patients’ and caregivers’ experiences with multidisciplinary or serial care. However, our participants were demographically, socioeconomically, and geographically diverse, to help achieve diversity of perspectives. In addition, following the standards of Grounded Theory, we continued conducting focus groups until we reached the point of thematic saturation, when no new information was being discovered (15).
Although we broadly solicited subjects, it is possible that participants were skewed towards advocates of the multidisciplinary model; our findings may not be applicable to other patient and caregiver populations; lung cancer patients and caregivers may have different feelings towards their care than those with other types of cancer; the providers associated with this particular multidisciplinary clinic may have appealed to the participants, so findings may be based on a provider effect, and not a model effect. However, our questions were open-ended, covered a wide range of topics, and elicited feedback on a variety of care logistics. Participants discussed infrastructural and efficiency benefits, including the value of the central point of contact, nurse navigation, and flexible but timely scheduling and referrals. This suggests that the favorable perceptions are generic.
Additional work is needed to critically examine the barriers to developing multidisciplinary care programs and to develop meaningful performance benchmarks for such programs from the perspectives of other key stakeholders, such as the different involved healthcare providers, institutional administrators, third party payers, and healthcare policymakers. These efforts will enable optimal development of multidisciplinary care programs that are feasible, effective, and sustainable within the usual practice environments where the majority of patients receive care for lung cancer.
Acknowledgements
This work was (partially) supported through a Patient-Centered Outcomes Research Institute (PCORI) Award (IH-1304-6147).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
References
- SEER Stat Fact Sheets: Lung and Bronchus Cancer. Available online: http://seer.cancer.gov/statfacts/html/lungb.html. Accessed July 21, 2015.
- Little AG, Gay EG, Gaspar LE, et al. National survey of non-small cell lung cancer in the United States: epidemiology, pathology and patterns of care. Lung Cancer 2007;57:253-60. [PubMed]
- Boffa DJ, Allen MS, Grab JD, et al. Data from The Society of Thoracic Surgeons General Thoracic Surgery database: the surgical management of primary lung tumors. J Thorac Cardiovasc Surg 2008;135:247-54. [PubMed]
- Ettinger DS, Wood DE, Ackerley W, et al. NCCN Guidelines®. Non-small cell lung cancer. Version 7.2015. Available online: http://www.nccn.org/professionals/physician_gls/pdf/nsclc.pdf, accessed July 21, 2015.
- BTS recommendations to respiratory physicians for organising the care of patients with lung cancer. The Lung Cancer Working Party of the British Thoracic Society Standards of Care Committee. Thorax 1998;53 Suppl 1:S1-8. [PubMed]
- Salomaa ER, Sällinen S, Hiekkanen H, et al. Delays in the diagnosis and treatment of lung cancer. Chest 2005;128:2282-8. [PubMed]
- Ost DE, Niu J. Quality gaps and comparative effectiveness in lung cancer staging and diagnosis. Chest 2014;145:331-45. [PubMed]
- Formulating new rules to redesign and improve care. In: Committee on Quality of Health Care in America, Institute of Medicine, editors. Crossing the Quality Chasm. A new health care system for the 21st century. Washington, DC: National Academy Press, 2001:61-88.
- ASCO-ESMO consensus statement on quality cancer care. J Clin Oncol 2006;24:3498-9. [PubMed]
- Tattersall MH. Multidisciplinary team meetings: where is the value? Lancet Oncol 2006;7:886-8. [PubMed]
- Leo F, Venissac N, Poudenx M, et al. Multidisciplinary management of lung cancer: how to test its efficacy? J Thorac Oncol 2007;2:69-72. [PubMed]
- Keating NL, Landrum MB, Lamont EB, et al. Tumor boards and the quality of cancer care. J Natl Cancer Inst 2013;105:113-21. [PubMed]
- Osarogiagbon RU, Robbins ET. Regional multidisciplinary thoracic oncology program comes to the Mid-South. Memphis Medical Society Quarterly 2013;15:12-3.
- Creswell JW, editor. Research design: qualitative, quantitative, and mixed methods approaches (3rd ed.). Los Angeles: Sage Publications, 2009:128-50.
- Strauss A, Corbin JM, editors. Basics of Qualitative Research. Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage Publications, 1998:116-42.
- Lincoln YS, Guba EG, editors. Naturalistic Inquiry. Thousand Oaks, CA: Sage Publications, 1985:289-331.
- Ballinger C. Demonstrating rigour and quality. In: Finlay L, Ballinger C, editors. Qualitative Research for Allied Health Professionals: Challenging Choices. Chichester, GB: John Wiley and Sons, 2006:235-46.
- Alberts WM, Bepler G, Hazelton T, et al. Lung cancer. Practice organization. Chest 2003;123:332S-337S. [PubMed]
- Fleissig A, Jenkins V, Catt S, et al. Multidisciplinary teams in cancer care: are they effective in the UK? Lancet Oncol 2006;7:935-43. [PubMed]
- Swanson PL, Strusowski P, Asfeldt T, et al. Expanding multidisciplinary care in community cancer centers. In: 2012 NCCCP Monograph; 2012:40-44. Available online: http://www.nxtbook.com/nxtbooks/accc/ncccp_monograph/#/42
- Look Hong NJ, Gagliardi AR, Bronskill SE, et al. Multidisciplinary cancer conferences: exploring obstacles and facilitators to their implementation. J Oncol Pract 2010;6:61-8. [PubMed]
- Devitt B, Philip J, McLachlan SA. Team dynamics, decision making, and attitudes toward multidisciplinary cancer meetings: health professionals’ perspectives. J Oncol Pract 2010;6:e17-20. [PubMed]
- Fujinami R, Otis-Green S, Klein L, et al. Quality of life of family caregivers and challenges faced in caring for patients with lung cancer. Clin J Oncol Nurs 2012;16:E210-20. [PubMed]
- Mosher CE, Jaynes HA, Hanna N, et al. Distressed family caregivers of lung cancer patients: an examination of psychosocial and practical challenges. Support Care Cancer 2013;21:431-7. [PubMed]
- Berwick DM. A user’s manual for the IOM’s ‘Quality Chasm’ report. Health Aff (Millwood) 2002;21:80-90. [PubMed]


