Targeted drugs in small-cell lung cancer
Introduction
Small-cell lung cancer (SCLC) accounts for approximately 15% of all newly diagnosed lung cancer cases and is strongly correlated with cigarette smoking. SCLC is morphologically and histologically distinct from non-small-cell lung cancer (NSCLC), extremely aggressive and is characterized by rapid doubling time, high growth fraction and early metastatic spread (1-3). Extension of the disease is considered the main prognostic factor and, based on this, SCLC is divided into limited-stage (LS-SCLC-confined to the thorax in a single radiation field) and extensive-stage disease (ES-SCLC-spread beyond the ipsilateral lung and regional lymph nodes and cannot be included in a single radiation field). The majority of patients are diagnosed with ES-SCLC, with metastases commonly observed in the contralateral lung and distant organs (4). Patients with limited disease are generally treated with platinum-based chemotherapy in combination with radiotherapy, which achieves a 15% to 20% cure rate. In recent years, the only advances in the management of SCLC have been in the field of radiotherapy where chest and prophylactic cranial irradiation have been demonstrated to significantly increase survival (3,5). For ES-SCLC patients, chemotherapy alone, represented by 4 to 6 cycles of cisplatin or carboplatin and etoposide, is the standard front-line treatment. Irinotecan plus platinum is an alternative option, especially outside the United States. Despite high initial responses to chemotherapy, patients inevitably develop drug resistance and relapse, sometimes rapidly, and succumb to the disease at a median of 10 to 12 months after diagnosis (1,2,5). Two-year survival for these patients is less than 5%. After relapse, single-agent topotecan is considered the standard second-line treatment, showing an improvement in overall survival (OS) compared with best supportive care (26 versus 14 weeks) and less toxicity than the combination regimen of cyclophosphamide, doxorubicin and vincristine (CAV) (5-7). Similar to other second-line therapies, treatment outcome to topotecan is generally better in those patients with longer disease control after first-line platinum based therapy. Other drugs, including taxanes, vinorelbine and gemcitabine, have demonstrated activity in this setting but have failed to show better survival outcomes compared to topotecan. Recent data suggest a role for temozolomide, mainly in those patients with central nervous system lesions and methylated methylguanine-DNA methyltransferase (8). Because of this dismal prognosis, there is an urgent need to develop novel, more specific and effective therapies for SCLC. Molecularly-targeted therapies have been demonstrated to be successful for treatment of advanced NSCLC. Molecular profiling of NSCLC has been introduced into routine clinical practice since the presence of specific oncogenic alterations, including epidermal growth factor receptor (EGFR) gene mutations and anaplastic lymphoma kinase (ALK) rearrangements, can be useful to guide treatment selection for specific subgroups of patients. Because of the limited therapeutic options and the poor survival of SCLC patients, several promising targeted agents have been developed on the basis of the growing number of molecular abnormalities identified for this cancer. However, despite numerous clinical trials, none has provided robust and practice-changing results and, to date, there are no currently approved targeted agents for this lung cancer subtype. Herein, we focus on reported results from the main clinical trials and future developments in targeted approaches aimed to improve therapeutic management of SCLC.
Molecular alterations in SCLC
SCLC is characterized by genomic instability and very high mutation load consistent with the effects of long-term exposure of DNA in cells to the carcinogens found in tobacco smoke (9). Genomic characterization of SCLC has been complicated by the difficulty in obtaining sufficient tumor tissue for analyses since this aggressive cancer is usually diagnosed at unresectable stages in small biopsies or cytology specimens. The development of patient-derived xenograft (PDX) models has made a huge contribution to deeper understanding of SCLC biology, especially characterization of driver mutations. The typical alterations found in SCLC are the nearly uniform loss of function of the tumor suppressors TP53 and RB1, which have long been described and confirmed in recent comprehensive genomic studies (1,10-16). In addition, a high frequency of deletions in chromosome 3p, which contains several tumor suppressor genes, has been reported (17). Loss of TP53, found in 75–90% of patients, could represent an important early event in SCLC tumorigenesis. The p53 protein has been described as “the guardian of the genome” because of its crucial role in maintaining genomic integrity after DNA damage by inducing cell cycle arrest or apoptosis and regulating the activity of DNA repair mechanisms. Moreover, recent studies have highlighted roles for p53 in modulating many other cellular processes, including metabolism, stem cell maintenance, invasion and metastasis, as well as communication within the tumor microenvironment (18). Loss of p53 function determines a condition of genomic instability and alteration of DNA repair mechanisms, which could be the molecular basis for further development and accumulation of key somatic driver mutations. Recently, whole-genome sequencing of 110 SCLC samples revealed the presence of somatic genomic rearrangements in TP73, another p53 family member, resulting in an oncogenic version of this gene, TP73Δex2/3 (14,19).
The retinoblastoma (RB1) is a tumor suppressor gene first identified in retinoblastoma that is inactivated in nearly all SCLCs (12,13). The product of this gene is a protein that plays an important role in regulation of the cell cycle (mainly in transition from G1 to S phase), apoptosis and cellular differentiation (20,21). In mice models, inactivation of TP53 and RB1 in respiratory epithelial cells resulted in the development of tumors closely resembling human SCLC, thus suggesting the key role of these genes in SCLC tumorigenesis (22).
Loss of RB1 has been also associated with upregulation of enhancer of zeste 2 (EZH2), a histone methyltransferase which is a core member of the polycomb repressive complex 2 (PRC2) and promotes cancer by epigenetically silencing tumor suppressor genes. It is also known to regulate Ras and p65/RelA (a measure of NF-κB activity). SCLC is characterized by extreme plasticity and cloning capacity consistent with a high degree of stemness. EZH2 expression was shown to regulate the proliferation of neural stem cells and the phenotypic switch between basal and secretory cells in lung epithelium, suggesting its expression is associated with increased cell plasticity (19,23). EZH2 was shown to be functionally active in SCLC tumors, exerting pro-tumorigenic functions in vitro, and was associated with aberrant methylation profiles of PRC2 target genes indicative of a “stem-cell like” profile in SCLCs (24). EZH2 can promote tumorigenesis by regulating cell cycle and apoptosis in SCLC cell lines (25). In our previous study, BRCA1 mRNA expression was significantly correlated with EZH2 and Musashi-2, another gene involved in stem cells’ self renewal and differentiation that regulates the Notch pathway via inhibition of Numb mRNA translation. Higher expression of EZH2 and BRCA1 were found in SCLC samples (26).
RB1 also binds directly to pluripotency genes, such as Oct4 and SOX2. In a comprehensive genomic study using next-generation sequencing technologies to characterize 36 primary SCLC tumors and 17 SCLC cell lines, SOX2 amplification was found in approximately 27% of samples. Suppression of SOX2 using shRNAs blocked proliferation of SOX2-amplified SCLC lines (16). Amplified SOX2 was first characterized as a driver oncogene in squamous lung cancer (27). SOX2 is a member of a large family of transcription factors involved in the maintenance of embryonic stem cells, induction of pluripotent stem cells and lung development; when overexpressed, it leads to tumorigenesis, including SCLC (28). In the same study, RNA sequencing identified multiple fusion transcripts and a recurrent RLF-MYCL1 fusion in 9% of SCLCs. Silencing of MYCL1 in SCLC cell lines that had the RLF-MYCL1 fusion decreased cell proliferation, suggesting its role as a key driver oncogene (16).
MYC is amplified in 20–30% of SCLC cases (29). The MYC family proteins, MYC, MYCN and MYCL, are transcriptional factors activated by numerous upstream intracellular pathways and regulating expression of a large number of genes involved in cell cycle and cell growth. The precise role of MYC in SCLC development or progression is not fully understood, however its role in the control of pluripotency, self-renewal, and epithelial-to-mesenchymal transition (all processes involved in neoplastic transformation) (19) it is well recognized. The phosphatidylinositol-3-kinase (PI3K)/AKT/mTOR signaling pathway, which regulates cell proliferation and growth as well as many other cellular functions, is commonly deregulated in several cancer types. Therefore, the pathway has been largely exploited for cancer drug discovery (30). The constitutive activation of the PI3K/AKT/mTOR pathway is also observed in a significant percentage of SCLC cases, as a result of alterations affecting key genes in the pathway, such as deletions of PTEN, PIK3CA mutations, or mTOR overexpression (15,16,19,31). By performing whole exone sequencing and copy number analysis on surgically resected SCLCs, genetic alterations in the PI3K/AKT/mTOR pathway were detected in 36% of the tumors and the individual changes in this pathway were mutually exclusive, suggesting the key driving role of each of the genes (31). The activation of the PI3K/AKT/mTOR pathway in SCLC has been correlated with aberrant cell proliferation and survival and resistance to chemotherapy, including platinum-compounds and radiotherapy (32,33). SCLC cell lines with genetic alterations in the PI3K/AKT/mTOR pathway did not show apparent cisplatin-mediated cytotoxicity but treatment with specific inhibitors (BEZ235, BKM120, INK128, MK2206) significantly impaired tumor cell proliferation (31).
Inactivating mutations in NOTCH family genes have been identified by whole-genome sequencing in 25% of human SCLC tumors, suggesting these alterations may represent a major feature of SCLC (14). NOTCH signaling is critical in regulation of the neuroendocrine compartment size in lung development and its inactivation could therefore contribute to malignant transformation of neuroendocrine cells. In fact, in the same study, activation of NOTCH signaling led to significantly fewer tumors and prolonged survival in SCLC transgenic mouse models (14,19).
Up-regulation of anti-apoptotic signaling pathways can also occur in SCLC. Specifically, the anti-apoptotic protein BCL-2 is overexpressed in SCLC cell lines and primary tissues and inhibits the proapoptotic proteins BAX and BAK. Overexpression of BCL-2 may be possibly correlated to loss of p53, which transcriptionally regulates BCL-2 (34-36). SCLC is a highly vascularized tumor and angiogenesis is essential for growth and early metastatic spread. SCLC expresses functional VEGF receptors, VEGFR-2 and VEGFR-3 (37), and VEGF has been associated with poor outcome in SCLC patients (38).
Although infrequently, other genes can also be altered in SCLC, including those encoding for receptor tyrosine kinases (RTKs), such as FGFR, EGFR, KIT, insulin-like growth factor 1 receptor (IGF-1R) and MET. The alterations affecting RTKs include overexpression, somatic gene mutations and gene amplification (15,39-46).
In 122 cases of SCLC patients, including 102 specimens obtained by biopsy and 20 from surgical resection, EGFR mutations were detected in five SCLCs (4%) (39). Patients with EGFR mutations were more likely to have SCLC combined with adenocarcinoma compared with the overall SCLC population. In three tumors with the combined SCLC subtype, both components of adenocarcinoma and SCLC had an EGFR mutation. In the very appealing study by Peifer et al., that performed integrative genome analyses on resected SCLC specimens, FGFR1 amplifications were found to occur in 6% of SCLCs (15). Preclinical data suggest that FGFR1 amplification is a driver oncogene in SCLC. Indeed, PD173074, a selective FGFR inhibitor, blocks SCLC growth both in vitro and in vivo (40). FGFR1 protein and messenger RNA (mRNA) expression and amplification, and also expression of its specific ligands, FGF2 and FGF9, were analyzed in primary tumors from 90 SCLC patients. FGFR1 protein expression was identified in 7% of cases and demonstrated a significant correlation with FGFR1 mRNA levels and FGFR1 gene amplification. FGFR1 mRNA expression also correlated with both FGF2 and FGF9 protein and mRNA expression. These results suggest the potential activation of the FGF/FGFR1 pathway in subset of SCLCs, which can be potentially targeted by specific inhibitors (41). Similarly to SOX2 amplification, amplified FGFR1 was first discovered and functionally validated as a driver oncogene in squamous lung cancer, highlighting that some genomic aberrations can overlap among different lung cancer subtypes (28).
The c-KIT protein is a member of the type III RTK family. High levels of expression of c-KIT and its ligand, the stem cell factor (SCF), have been widely found in SCLC tumors (42). Abnormal expression of c-KIT may be involved in pathogenesis of SCLC by autocrine/paracrine stimulation of the SCF/c-KIT signaling pathway. In a retrospective analysis of 203 SCLC patients, expression of c-KIT by immunohistochemistry was observed in 87.7% of SCLC tumor samples and was an independent prognostic factor (43). The insulin-like growth factors (IGF) and their receptors play fundamental roles in cellular signaling transduction and regulate cell growth, differentiation, apoptosis, transformation and other important physiological processes. The IGF-1R is mainly involved in the activation of the Ras/mitogen-activated protein kinase (MAPK) pathway and PI3K/AKT pathway, and also forms cross-talk with the EGFR pathway. Insulin-like growth factor-I (IGF-I) is a potent autocrine growth factor for SCLC. The IGF-1R has also been demonstrated to be over-expressed in SCLC (44).
Aberrations in epigenetic regulators have been found to be a major feature of SCLC. Indeed, recurrent mutations in genes encoding histone modifiers such as the histone acetyltransferases (HATs) CREBBP and EP300 and the histone methyltransferases MLL, MLL2 and EZH2 have been described in comprehensive genomic studies in SCLC tumor samples (15,16,47,48). Using an integrative proteomic and transcriptomic analysis, SCLCs showed significantly increased levels of EZH2, thymidylate synthase, apoptosis mediators, and DNA repair proteins, including the PARP1, a DNA repair protein and E2F1 co-activator that was highly expressed at the mRNA and protein levels. SCLC growth was inhibited by PARP1 and EZH2 knockdown (47). The Hedgehog (Hh) signaling pathway is involved in embryonic development of the airway epithelium by regulation of morphogenesis and stem-cell fate. Abnormal activation of this pathway also plays a significant role in SCLC development and progression. Constitutive activation of the Hh signaling molecule Smoothened (Smo) promoted clonogenicity of human SCLC in vitro and initiation and progression of mouse SCLC in vivo. Pharmacological inhibition of this signaling inhibited growth of human and mouse SCLC models, most notably following chemotherapy (49).
Targeted agents tested in SCLC
Receptor tyrosine kinases (RTKs) inhibitors
Several compounds targeting specific RTKs have been developed and tested in clinical trials in SCLC patients (Table 1). Imatinib mesylate (STI571) is an oral small molecule inhibitor of tyrosine kinase activity of c-kit which acts through occupation of the ATP binding site within the TK domain. Its activity is associated with the presence of activating mutations of the KIT gene at exons 9 and 11, which are commonly observed in gastrointestinal stromal tumors (GISTs) (50). Imatinib was evaluated in pre-clinical studies in SCLC as single-agent or in combination with chemotherapy (51,52). However, in different phase II studies, imatinib mesylate has failed to demonstrate significant clinical activity in SCLC as monotherapy as well as in combination with chemotherapy in previously untreated patients or in the maintenance setting following chemotherapy (53-57). The cause of these negative results may be due to the low incidence of KIT exon 9 or 11 mutations in SCLC, as reported in some studies (58,59).
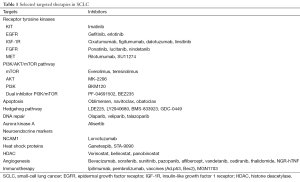
Full table
The efficacy of EGFR tyrosine kinase inhibitors (TKIs), including gefitinib, erlotinib and afatinib, has been widely established in patients with EGFR-mutant NSCLC (60). However, they have failed to show significant clinical benefit for treatment of unselected patients with relapsed SCLC (61). These negative results are most likely explained by the rarity of EGFR mutations in SCLC. EGFR mutations may occur more frequently in histological combined subtypes of SCLC with adenocarcinoma and gefitinib and erlotinib have demonstrated some activity in these subgroups (39). Therefore, selection of molecularly-defined subgroups of patients could improve outcomes with these small molecule TKIs and oncogene-directed therapeutic approaches need further evaluation.
IGF-I/IGF-1R signaling activation has been shown to inhibit chemotherapy-induced apoptosis through PI3K/AKT pathway, and inhibition of this signaling pathway can sensitize SCLC to the cytotoxic effects of chemotherapy and radiotherapy in preclinical models (62,63). Small molecule inhibitors of the IGF-1R tyrosine kinase, such as linsitinib (OSI-906), and humanized monoclonal antibodies, including cixutumumab and dalotuzumab (MK-0646), are currently being studied in ongoing clinical trials in SCLC (NCT00887159, NCT1533181, NCT00869752) (Table 1) (64). A phase II trial of the monoclonal antibody figitumumab in association with cisplatin (or carboplatin) and etoposide as first line treatment of extensive disease SCLC was terminated prematurely due to low participants enrollment and the halting of the figitumumab development program (NCT00977561). Some potential molecular biomarkers of response to IGF-1R inhibitors have been investigated to better select patients for treatment. IGF-1R, IR, IGF-1 and -2, IGFBP3 and IGFBP6 expression did not correlate with sensitivity of SCLC cell lines to OSI-906. In contrast, lower baseline phospho-ERK levels were shown in OSI-906 sensitive line compared to resistant-cells. OSI-906 exposure resulted in a concentration-dependent decrease in phospho-IGF-1R and phospho-Akt in sensitive and resistant lines, but induced cell cycle arrest and apoptosis only in sensitive lines. Therefore, IGF-1R inhibitors may be effective therapies for a SCLC subset with low pre-treatment phospho-ERK levels (65).
Targeting the FGFR1, which is amplified in 5–6% of SCLCs (15,66) may represent a promising therapeutic approach and FGFR pathway inhibition represents an active area of investigation in SCLC. PD173074, a small and potent molecule inhibitor of FGFR, blocked SCLC growth in vitro and in vivo (40). Molecular alterations of different members of the FGF/FGFR1 pathway have been described and can affect response to specific inhibitors (41). The FGFR inhibitor ponatinib is currently being studied in a biomarker driven trial in lung cancer (NCT01935336). A phase II trial to assess the efficacy and safety of lucitanib, which targets FGFR1-3, VEGFR1-3, and PDGFRα/β and has both anti-tumor and anti-angiogeneic activity, in advanced lung cancer (both NSCLC and SCLC) with FGF, VEGF and PDGF genetic alterations, is currently ongoing (NCT02109016). BIBF1120, a multitargeted drug that inhibits FGFR, VEGFR and PDGFR is also under clinical evaluation (NCT01703481, NCT01441297).
The RTK c-MET is also expressed in SCLC. c-MET ant its ligand, hepatocyte growth factor (HGF), regulate numerous cellular processes that stimulate cell proliferation, invasion and angiogenesis (42,45). Activating mutations of c-MET, although relatively rare, can also be found in SCLC. However, in the study by Voortman et al, these mutations did not influence c-MET phosphorylation and its inhibition by specific TKI treatment (46). In another study in MET mutant SCLC cells, HGF induced MET phosphorylation, increased proliferation, invasiveness and clonogenic growth. The MET inhibitor PHA-665752 blocked MET phosphorylation and counteracted HGF-induced effects. Phosphorylation of MET in clinical samples was correlated with poor prognosis (67). MET can be effectively inhibited by small molecules and monoclonal antibodies (Table 1). In pre-clinical studies in SCLC cell lines, the small molecule MET inhibitor SU11274 was found to synergize with the Top1 inhibitor SN-38 (68). Rilotumumab (AMG 102) is a fully human MAb (IgG2) that specifically targets HGF. It binds to aminoacid residues at the NH2-terminus of the β-chain of human HGF, with a preference for the mature, heterodimeric form. A multicenter, phase Ib/II trial of AMG 102 in combination with platinum-based chemotherapy as first-line treatment for extensive stage SCLC has completed accrual (NCT00791154).
PI3K/AKT/mTOR pathway inhibitors
Due to the key role of PI3K/AKT/mTOR pathway activation in mediating aberrant cell proliferation and survival and resistance to chemotherapy and radiotherapy in SCLC, a number of inhibitors of single key components of the pathway, including PI3K, AKT and mTOR, have been developed in recent years. Some of these inhibitors have demonstrated promising activity and induce reversal of chemoresistance in pre-clinical studies (33,45,69-72). Different rapamycin analogs have been tested in clinical trials in SCLC patients, however results have reported only limited clinical activity. In a phase II study, everolimus administered as single agent in previously treated, relapsed SCLC, showed limited activity, with a disease-control rate at six weeks of 26% (95% CI, 11–40%), only one partial response observed and a median progression-free survival (PFS) of 1.3 months. However, the drug demonstrated manageable toxicity (73). In a phase Ib study, 21 previously-treated SCLC patients received everolimus at three different doses in combination with paclitaxel. At the dose of 5 mg once daily in combination with paclitaxel, everolimus showed an acceptable safety profile and an overall objective response rate of 28% (74). However, in a phase Ib dose-escalation study in the first-line setting of extensive-stage SCLC patients, the combination of different doses of daily or weekly everolimus with cisplatin and etoposide was associated with excessive hematological toxicity. Indeed, grade 3/4 febrile neutropenia occurred in 40% of patients receiving daily everolimus and for this reason, the protocol was amended to introduce the use of prophylactic granulocyte colony-stimulating factor (G-CSF). Everolimus 2.5 mg/day plus G-CSF was the only feasible dose given with standard-dose chemotherapy and was associated with a disease control rate of 58.3% (nine of 12 patients evaluable for response). Although showing a promising PFS of 8.1 months, everolimus plus etoposide did not seem to substantially improve tumor response compared with etoposide alone (75). The identification of biomarkers which can predict sensitivity or resistance to everolimus and other mTOR inhibitors could be helpful to select patients for treatment and could also suggest novel potential drug combinations to improve their efficacy in the clinical setting. In a previous study, everolimus was particularly active in a subset of SCLC cell lines with PI3K/AKT pathway activation and low BCL-2 expression (71). Interestingly, the limited, single-agent activity of the BH3-mimetic drugs ABT-737 and ABT-263 can be rescued by mTOR inhibitors in SCLC, as demonstrated in in vitro and in vivo preclinical studies (76,77). Recently, MYC and the eukaryotic translation initiation factor 4E (eIF4E) were found to be overexpressed in everolimus-resistant SCLC cells. Interestingly, after reduction of MYC or eIF4E by siRNAs, some resistant cells displayed increased sensitivity to everolimus, suggesting their contribution to determining resistance to the mTOR inhibitor. Therefore MYC-eIF4E and mTOR inhibitors can represent a new potential therapeutic combination (78). In pre-clinical studies, erlotinib with everolimus was demonstrated to have synergistic effects on SCLC cell viability, proliferation and autophagy (79). AKT inhibitors are also under investigation. In a phase II trial the AKT inhibitor MK-2206 is being evaluated in those cancers (advanced NSCLC, SCLC and thymic malignancies) harboring PIK3CA mutations or amplification, AKT or PTEN mutations (NCT01306045). A phase I trial of the PI3K inhibitor BKM120 in combination with cisplatin and etoposide in advanced solid tumors and SCLC is also ongoing (NCT02194049). Dual inhibitors of PI3K and mTOR, such as BEZ235 and PF-04691502, could represent the most promising drugs, since they have been demonstrated to inhibit the pathway at multiple levels, also blocking a possible reactivation that can result in drug resistance, and are currently being evaluated in phase I studies in advanced cancer patients (NCT01195376, NCT00927823).
Agents targeting apoptosis
Triggering cell apoptosis is one of the most promising therapeutic anti-cancer approach since several cancer types, including SCLC, are characterized by overexpression of antiapoptotic BCL-2 family members, the molecular sentinels of apoptosis (34-36). Inhibition of BCL-2 increased the efficacy of cisplatin and etoposide in human SCLC lines in tissue culture and in murine xenografts, suggesting this combination may significantly increase the antitumor efficacy of cytotoxic chemotherapy alone (80). Different BCL-2 family inhibitors, including antisense oligonucleotides (e.g., oblimersen), ABT-737, navitoclax (ABT-263) and obatoclax (CX15-070), have been tested in clinical trials in SCLC. Oblimersen (G3139) is an antisense oligonucleotide complementary to the first six codons of the BCL-2 mRNA, and represents the first targeted BCL-2 inhibitor tested in clinical trials. It has demonstrated synergy with cytotoxic agents in preclinical models and good tolerability in phase I trials in combination with standard chemotherapy (81,82). A randomized phase II trial was conducted to assess the efficacy and toxicity of carboplatin and etoposide with or without oblimersen, as first line therapy for extensive-stage SCLC. The results showed no benefit in terms of response rate, failure-free survival and OS for the oblimersen arm, but higher grade 3 to 4 hematologic toxicity, compared to chemotherapy alone (83).
Obatoclax mesylate is a small-molecule BH3-mimetic that disrupts the dimerization between anti-apoptotic factors such as BCL-2, BCL-XL and MCL-1 and pro-apoptotic proteins such as BAX and BAK. Obatoclax exerts cytotoxic effects across a range of solid tumor cell lines and xenograft models and has been shown to synergize with conventional cytotoxic chemotherapy (84,85). A randomized, phase II trial evaluated the efficacy and safety of obatoclax in combination with carboplatin and etoposide for the treatment of extensive-stage SCLC patients. The primary endpoint was objective response rate and this was higher for the obatoclax and chemotherapy arm (62%) compared to chemotherapy alone (53%), although not statistically significant (P=0.143). Obatoclax in combination with chemotherapy was well tolerated but failed to significantly improve PFS and OS (86). In a previously reported open-label, phase II study, the addition of obatoclax to topotecan in patients with relapsed SCLC showed a lack of benefit in terms of overall response rate (ORR). Indeed, of nine patients enrolled, no responses and only five stable diseases were observed (87).
Navitoclax (ABT-263) is a BH3 mimetic that directly binds BCL-2 and BCL-XL, blocks their binding to BIM and thereby enables BIM-mediated induction of apoptosis. However, ABT-263 does not bind the prosurvival BCL-2 family member myeloid cell leukemia 1 (MCL-1). Navitoclax was demonstrated to be well tolerated and have preliminary encouraging efficacy in a phase I study (88), but showed limited activity in a phase II trial in which it was administered as single agent in pre-treated patients with recurrent and progressive SCLC. In this study, among 39 patients enrolled, partial response was observed in only one patient (2.6%) and stable disease in nine (23%) (89). Exploratory analyses suggested some potential predictive biomarkers, including plasma baseline levels of cytokeratin 19 fragment antigen 21-1, which was also correlated with tumor BCL-2 copy number, neuron-specific enolase, pro-gastrin-releasing preptide (pro-GRP), and circulating tumor cell (CTC) number (89). In a very recent, interesting study, SCLC cell lines with higher expression of the proapoptotic gene Bcl2-interacting mediator of cell death (BIM) showed higher sensitivity to the BH3-mimetic drug navitoclax. However, some cells are relatively resistant due to high expression of the antiapoptotic MCL-1, which is able to sequester BIM and abrogate apoptosis. The combination of the mTOR inhibitor ZD8055 and ABT-263 induced marked apoptosis in cell lines and significant tumor regressions in multiple SCLC xenograft models, probably because mTORC1/2 inhibition is able to reduce the expression of MCL-1 (77). Therefore, this study suggests a new synergistic combination therapy for SCLC including BCL-2 and mTOR inhibitors.
Hedgehog (Hh) pathway inhibitors
Hh pathway signaling activation has been revealed in airway development during normal differentiation of pulmonary neuroendocrine precursor cells and in a subset of SCLC, which is known to have primitive neuroendocrine features. These tumors maintain their malignant phenotype in vitro and in vivo through ligand-dependent Hh pathway activation (90). Constitutive activation of the Hh signaling molecule Smo promoted clonogenicity of human SCLC in vitro and the development and maintenance of mouse models of SCLC in vivo. In the same study, pharmacological inhibition of Hh signaling inhibited the growth of mouse and human SCLC (49). Notably, treatment was highly effective in preventing the recurrence of residual tumors following chemotherapy, suggesting a synergistic role between the Hh pathway and chemotherapy (49). Several inhibitors of components of this pathway, including LDE225 and LY2940680, are currently being investigated in early phase trials in patients with extensive stage SCLC in combination with chemotherapy (NCT01579929, NCT1722292) (45). A phase Ib multiple ascending dose study to evaluate the safety and phamarcokinetics of BMS-833923 (XL139) with carboplatin and etoposide followed by BMS-833923 in patients with extensive stage SCLC has been completed and results are pending (NCT00927875). Vismodegib (GDC-0449) is an orally bioavailable small molecule that targets the Hh signaling pathway, blocking the activities of the Hh-ligand cell surface receptors PTCH and/or SMO and suppressing Hh signaling. The drug is approved for treatment of basal-cell carcinoma. A randomized phase II study has been carried out to test cisplatin and etoposide in combination with either the Hh inhibitor vismodegib or with the anti-IGF-1R monoclonal antibody cixutumumab (IMC-A12) for patients with extensive stage SCLC, with PFS as the primary endpoint (NCT00887159). Those patients with stable disease or responses after four cycles of concomitant treatment were continued on vismodegib or cixutumumab until disease progression. One hundred and fifty-five patients were eligible for treatment. Although the combinations were fairly well tolerated, no statistically significant improvement in PFS or OS with the addition of either targeted agents to chemotherapy versus chemotherapy alone was observed. Median OS was higher for patients with low CTCs count at baseline compared to those with high CTC count (91).
Agents targeting DNA repair alterations
A network of complementary DNA repair systems is activated in normal cells to process DNA damage caused by endogenous and environmental factors, thus maintaining genomic integrity and suppressing tumorigenesis (92). Platinum-compounds, the backbone of SCLC treatment, cause harmful DNA cross-links which interfere with DNA repair mechanisms and induce DNA damage. Similar to other solid tumors, SCLC is characterized by genomic instability and dysfunctional DNA repair mechanisms can contribute to this feature. Targeting DNA repair itself can also represent a novel therapeutic strategy for SCLC to increase cytotoxicity of anticancer agents, reverse chemotherapy resistance and improve therapeutic efficacy. Poly (ADP-ribose) polymerase (PARP1) is a key enzyme of the base excision repair (BER) system, specifically involved in DNA single-strand break (SSB) repair, and an E2F1 co-activator (93). By using an integrative proteomic and transcriptomic analysis, it was found that SCLC showed the highest expression of PARP1 at the mRNA and protein levels of all histological subtypes of lung cancers and was significantly more sensitive to PARP inhibitors than NSCLC. Inhibition of PARP in SCLC was shown to suppress the expression of several E2F1-regulated DNA repair proteins, including RAD51, which in turn may contribute to DNA repair deficiency and the sensitivity of SCLC to these drugs. PARP inhibition also enhanced chemotherapy efficacy (47). PARP inhibitors are strong radiation- and chemo-sensitizers in vitro (94). So far, the most successful application of the synthetic lethality concept in anti-cancer research has led to the discovery and development of PARP inhibitors to treat cancers with BRCA1 or BRCA2 mutations. Cells carrying BRCA mutations are up to 1,000 times more sensitive to PARP inhibitors than wild type cells (95).
Talazoparib (BMN 673) is a highly potent PARP1/2 inhibitor with selectivity for tumors with DNA repair defects, resulting in synthetic lethality. In preclinical study, BMN 673 demonstrated single agent activity in SCLC cell lines and xenografts. Sensitivity to BMN 673 was associated with elevated baseline expression levels of multiple DNA repair proteins (“DNA repair score”), whereas drug resistance was observed in SCLC models with baseline activation of the PI3K/mTOR pathway (96). BMN 673 showed single agent anti-tumor activity in a two-stage (dose-escalation and dose expansion) phase I study including patients with previously treated advanced SCLC and ovarian and breast cancer patients with germline mutations in BRCA1 and BRCA2. Partial responses were reported in 2/20 patients (10%) and clinical benefit (complete response, partial response and stable disease ≥16 weeks) in 5/20 (25%). The median duration of response was 13.7 weeks (95% CI, 12.0–15.3 weeks) (97). The drug was well tolerated, with the most common drug-related adverse events being myelosuppression, fatigue, nausea and alopecia.
Veliparib is also demonstrated to have limited activity as a single agent but significantly potentiated the cytotoxicity of standard chemotherapeutic agents, including platinum compounds and etoposide. Results from the phase I, dose-escalation part of a phase I/II clinical study including treatment-naïve, extensive stage SCLC patients have been recently reported (NCT01642251). In this study, veliparib at 100 mg in combination with cisplatin and etoposide at standard doses was selected as the recommended phase II dose. The combination was safe and of seven evaluable patients, there were four partial responses (57.1%) and one complete response (98). Further studies are needed to identify biomarkers that may predict response to these drugs, including levels of PARP1 or other DNA repair proteins.
MYC inhibition
Several strategies have been used to target MYC-dependent cells, including bromodomain inhibitors such as JQ1 that was able to lead to down-regulation of MYC-driven transcription, cell cycle arrest and senescence (19,99,100). By using a high-throughput cellular screen of a diverse chemical library it was observed that SCLC cell lines and mouse models were sensitive to transcription-targeting drugs, in particular to THZ1, a covalent inhibitor of cyclin-dependent kinase 7 (CDK7). The expression of super-enhancer associated transcription factor genes, including MYC, and neuroendocrine lineage-specific factors or SOX2 was associated with high vulnerability to THZ1 treatment, suggesting these could represent potential predictive markers of response to these inhibitors (101). Another strategy to indirectly target MYC is through the use of Aurora Kinase inhibitors.
Aurora kinases inhibitors
The Aurora kinases comprise a family of protein kinases that play a critical role in the mitotic process. Aurora A kinase (AURKA) localizes to the centrosomes and spindle poles and recruits the cyclin B1-CDK1 complex, committing the cell to mitosis. Amplification of AURKA is oncogenic and has been observed in some cancer types, including colorectal, gastric and breast cancer and can be associated with resistance to some mircotubule-disrupting cytotoxic agents, such as paclitaxel. Aurora B kinase plays an important role in chromosome condensation, regulation of kinetochore function, and cytokinesis. AURKA activity inhibition significantly arrests mitotic progression through activation of the mitotic checkpoint. In contrast, inhibition of Aurora B kinase drives the cell out of mitosis. In cells with a defective postmitotic checkpoint or those with uncontrolled cell-cycle entry, such as those with MYC overexpression or loss of function RB, incessant DNA replication leads to endoreduplication, causing cell death secondary to genomic instability (102). MYC-amplified tumors, including SCLCs, are particularly sensitive to inhibition of aurora kinase (103,104). Alisertib (MLN8237) is a selective, ATP-competitive and reversible small-molecule inhibitor of AURKA. In a multicenter, phase II trial in pre-treated patients with different advanced solid cancers, alisertib showed promising response rates as single-agent in recurrent SCLC. Among response-assessable patients, objective responses were noted in 10 (21%) of 48 participants with SCLC (105). The most frequent drug-related grade 3–4 adverse events included neutropenia, leukopenia and anaemia, and serious drug-related adverse events were reported in 43% of patients. Since AURKA has a critical role in controlling mitotic spindle assembly, specific AURKA inhibitors may be strongly active in combination with taxane. A randomized, double-blind, placebo-controlled, phase II study of alisertib (MLN8237) in combination with paclitaxel versus placebo as second line therapy for SCLC is currently ongoing (NCT02038647). SCLCs with MYC overexpression are those most likely to benefit from these specific targeted agents.
Histone deacetylase (HDAC) inhibitors
HDACs are enzymes involved in the remodeling of chromatin which play a key role in epigenetic regulation of gene expression. Remodeling of chromatin results from modifying the structure of nucleosomes which comprise a histone octamer around which DNA is wrapped. The opposing activities of HATs and HDACs tightly regulate expression of a large number of genes involved in the control of cell cycle and proliferation and many other cellular processes through chromatin modification (106). HATs transfer acetyl groups to amino-terminal lysine residues in histones, which results in local expansion of chromatin and increased accessibility of regulatory proteins to DNA, whereas HDACs catalyze the removal of acetyl groups, leading to chromatin condensation and transcriptional repression. The therapeutic potential of HDAC inhibitors stems from their capacity to selectively induce apoptosis in tumor cells. In preclinical studies, HDAC inhibitors, including romidepsin, valproate and panobinostat have been shown to inhibit SCLC cell growth in vitro and in vivo and improve efficacy of chemotherapy (45,107-109). Also, the combination of HDAC inhibitors and DNA methyltransferases has shown activity (110). Panobinostat (LBH589), a pan-deacetylase inhibitor, was tested in a phase II study in patients with previously treated SCLC. Although few cases showed tumor shrinkage and sustained stable disease and the drug had a favorable profile, the study was prematurely closed due to lack of activity (111). Belinostat is being tested in a phase I study in association with cisplatin and etoposide in recurrent or advanced cancers, including SCLC (NCT00926640).
Heat shock protein 90 (Hsp90) inhibitors
Hsp90 serves as molecular chaperone that regulates the folding, stabilization and function of a great number of client proteins with important cellular functions, including the products of activated oncogenes. Many cancers have increased expression of Hsp90, suggesting Hsp90 inhibition as a promising therapeutic target (112). In a recent preclinical study in SCLC cell lines, the Hsp90 inhibitor ganetespib synergized with both doxorubicin and etoposide, two cytotoxic drugs with well known activity in SCLC. Expression of RIP1, a pro-survival scaffold protein that mediates chemotherapy resistance, was induced by doxorubicin and downregulated by ganetespib. Ganetespib and doxorubicin combination significantly inhibited SCLC growth in vitro and in mouse xenograft models (113). A phase I/II study of ganetespib in combination with doxorubicin in solid tumors (phase I) and in relapsed SCLC (safety dose expansion, phase II) is currently ongoing (NCT02261805).
Anti-angiogenesis
Bevacizumab, a humanized monoclonal antibody targeting VEGF and approved for first-line treatment of advanced NSCLC, was evaluated in clinical trials in SCLC patients in different settings. Single-arm, phase II studies were carried out in untreated, extensive-stage SCLC patients and showed promising results without serious or new safety signals observed (114-116). The single-arm, phase II CALGB 30306 study was carried out to assess the efficacy of cisplatin and irinotecan in combination with bevacizumab in patients with untreated extensive-stage SCLC. Result in terms of efficacy outcomes was promising, with a median PFS of seven months, OS of 11.6 months and ORR 75%, including 5% of patients achieving a complete response. However, the trial did not meet the primary endpoint to improve 12-month survival rates (114). In the Eastern Cooperative Oncology Group (ECOG) 3501 study, patients with extensive stage SCLC received cisplatin and etoposide plus bevacizumab and ORR was 64%, median PFS 4.7 months and median OS 10.9 months (115). In the first pacebo-controlled, double-blind, randomized multicenter phase II clinical trial, bevacizumab added to first-line standard chemotherapy (etoposide plus carboplatin or cisplatin) for treatment of extensive-stage SCLC improved PFS (5.5 months compared to 4.4 months in the placebo group; HR, 0.53; 95% CI, 0.32–0.86), with an acceptable toxicity profile. However, no improvement in OS was observed (9.4 vs. 10.9 months for bevacizumab and placebo group, respectively; HR, 1.16; 95% CI, 0.66–2.04). As the authors commented, the trial was probably not powered to evaluate the impact on OS and no data about second-line treatments were collected. It is possible that imbalances in subsequent therapies might have confounded the ability of the study to demonstrate a survival difference between the two groups (117). An Italian multicenter, randomized phase III trial comparing combination cisplatin, etoposide and bevacizumab versus the same chemotherapy regimen alone in the first-line treatment of SCLC patients with extensive disease is ongoing, with OS as the primary endpoint (118). Also, in the second-line setting, the combination of bevacizumab with standard chemotherapy, topotecan or paclitaxel showed activity and promising PFS compared to historical controls in phase II, single-arm studies (119,120). A phase II study of bevacizumab in combination with cisplatin and etoposide and radiation for patients with limited-stage SCLC has completed accrual (NCT00387699). Other anti-VEGF/VEGFRs agents have been studied in SCLC, including mutikinase inhibitors with a broad spectrum of anti-tumor activity, such as sorafenib, sunitinib, cediranib, vandetanib and thalidomide (Table 1). A phase II trial of sorafenib in platinum-treated extensive stage SCLC failed to achieve disease control (121). A phase II study of cisplatin and etoposide plus concurrent and sequential sorafenib in patients with previously untreated SCLC was terminated early on the basis of excessive toxicity observed and preliminary efficacy data showing that study was unlikely to meet its primary endpoint (a 60% 1 year survival rate was expected with the addition of sorafenib, compared to 35% to 40% of the historical control) (122). The combination of sunitinib with standard chemotherapy seemed to cause prolonged neutropenia and an unacceptable rate of treatment-related mortality (123). A single-arm trial testing second-line sunitinib in SCLC reported a 9% partial response and 29% stable disease rate with significant toxicity (63% grade 3 or 4 thrombocytopenia and 25% neutropenia) (124). Different phase II trials evaluated maintenance sunitinib following first line platinum based chemotherapy for patients with extensive-stage SCLC, with conflicting results in terms of efficacy and toxicities, although some substantial differences existed among these trials and in sunitinb dosages (125-127). In the recently published CALGB 30504 study, maintenance sunitinib was safe and improved PFS compared to placebo (2.1 months for placebo and 3.7 months for sunitinib; HR, 1.62; 95% CI, 1.02–2.60; P=0.02) in extensive-stage SCLC (127). Cediranib failed to show objective responses in a phase II study in patients with progressive SCLC after one prior platinum-based regimen and the initial dose had to be reduced due to excessive grade 3/4 toxicities (128). Vandetanib as maintenance therapy in responding SCLC patients after chemotherapy failed to improve median survival times compared with placebo and was associated with more toxicities and dose modifications for gastrointestinal toxicity and rash (129).
Although showing promising results in early phase II trials, in a large, randomized phase III trial, thalidomide in combination with carboplatin and etoposide did not improve survival of patients with limited or extensive-stage SCLC and was associated with an increased risk of thrombotic events (130). In another randomized, double-blind, placebo-controlled phase III study of thalidomide in extensive-stage SCLC after response to chemotherapy, treatment with thalidomide was not associated with a significant improvement in survival (11.7 vs. 8.7 months, respectively; HR 0.74; 95% CI, 0.49–1.12; P=0.16) but with higher incidence of neuropathy (131). Currently, the regimen that was used in this trial, the PCDE (etoposide, cisplatin, cyclophosphamide and 4'-epidoxorubicin) is not a standard for SCLC patients, and other chemotherapy regimens, including etoposide and cisplatin combined with thalidomide, warrant of further investigation. Pazopanib is also being tested in ongoing trials in SCLC as maintenance therapy after platinum/etoposide first-line therapy (NCT01797874) and in previously treated patients with relapsed SCLC (NCT01713296, NCT01253369).
Other anti-angiogenetic therapies that have been tested include aflibercept (ligand-trap binding VEGF) and the NGR-hTNF (a recombinant protein specifically designed to act on tumor blood vessels). The addition of aflibercept to weekly topotecan as treatment of patients with progressive SCLC was tested in a randomized phase II trial. Patients were stratified according to response and treatment-free interval as either platinum sensitive (complete response or partial response and >90 day treatment-free interval for extensive stage or ≥180 days for limited stage) or platinum refractory (no response and/or treatment-free interval ≤90 days for extensive stage and <180 days for limited- stage). The 3-month PFS was significantly improved with the addition of aflibercept in patients who had platinum-refractory disease (27% vs. 10%; P=0.02) but not in patients with platinum-sensitive disease (24% vs. 15%; P=0.22). Disease control rate was higher with aflibercept in both groups of patients, no differences in OS were observed and the addition of aflibercept increased toxicity (132). NGR-hTNF, a new vascular targeting agent generated by the fusion of the CNGRCG peptide interacting with CD13 on blood vessels to the N-terminal do-main of murine (m) or human (h)TNF is currently being tested in several phase II-III trial in different tumor types. This drug can improve the intratumoral doxorubicin penetration by normalizing tumor vasculature and decreasing tumor interstitial fluid pressure. The combination of NGR-hTNF and doxorubicin was demonstrated to be safe in relapsed SCLC patients and showed evidence of antitumor activity and promising PFS which appeared to be weakly correlated with platinum-sensitivity in the subset analyses (133).
At the present, overall efficacy and safety results for angiogenesis inhibitors in SCLC suggest that careful selection of patients on the basis of reliable predictive biomarkers is urgently needed.
Immunotherapy
Melanoma and lung cancers show the highest mutation frequencies of all tumor types, which is probably related to exposure to well known carcinogens, such as UV radiation in the case of melanoma and tobacco smoke in the case of lung cancers (134). These mutations generate a variety of tumor-specific antigens that may contribute to increased lung cancer immunogenicity. In recent years, several immunotherapies have been developed and tested in lung cancer. To date, the most promising seem to be checkpoint inhibitors against the CTLA-4 and PD-1/PD-L1 pathway which counteract the mechanisms exploited by tumors to suppress and evade the immune system. A higher mutational load as assessed by whole-exome sequencing in NSCLC samples from patients was strongly associated with response to the anti-PD-L1 antibody pembrolizumab. Efficacy was also correlated with a molecular smoking marker, specific DNA repair pathway mutations, and a higher burden of candidate neoantigens (135-137). In addition to a very high mutational burden, SCLC is characterized by high expression of PD-L1 (138), suggesting that activation of the PD-1/PD-L1 is a major mechanism through which tumor cells escape immunosurveillance and that these cells can be particularly sensitive to the PD-1/PD-L1 pathway blockade. High PD-L1 expression has been also correlated with survival. Ipilimumab is a fully humanized IgG1 anti-CTLA-4 monoclonal antibody that blocks binding of CTLA-4 to its ligand, thus boosting antitumor immune responses. Ipilimumab was tested in a randomized, double-blind, multicenter phase II trial in extensive-disease SCLC patients in which it was combined with carboplatin and paclitaxel in a phased schedule (after chemotherapy) or in a concurrent schedule and compared with chemotherapy plus placebo (139). The rationale for the phased regimen was that chemotherapy could allow antigen release before initiation of immune modulation by ipilimumab. The primary end point was immune-related PFS (irPFS), assessed by immune-related response criteria and modified WHO criteria. Other end points included PFS, best ORR, OS and safety. Phased ipilimumab improved irPFS compared to control (6.4 vs. 5.3 months, HR, 0.64, P=0.03) but no statistically significant improvement in PFS or OS was observed (139). Ipilimumab is being tested in a phase III trial in SCLC in association with etoposide plus a platinum agent (NCT01450761). Preliminary safety and efficacy data in SCLC from an ongoing multi-cohort phase Ib study of pembrolizumab in patients with PD-L1 positive advanced solid tumors (KEYNOTE-028) after failure of standard therapy have been recently presented (140). The primary endpoints of this study are ORR by RECIST 1.1 and safety. Pembrolizumab showed promising anti-tumor activity in SCLC patients. The ORR was 35% (seven partial responses out of 20 evaluable patients). Median time to response was 8.6 weeks; responses were rapid and durable, with six of seven patients showing ongoing responses at data cutoff. Treatment toxicity was consistent with previous experience, with one treatment-related death from colitis (140). An ongoing phase II study is testing pembrolizumab in extensive stage SCLC patients as maintenance treatment following combination therapy (NCT02359019). A phase I study is testing pembrolizumab plus radiation therapy and combination chemotherapy (NCT02402920). Also a phase III trial is ongoing to test the other PD-1 inhibitor, nivolumab, versus topotecan as second line in advanced SCLC (CheckMate 331, NCT02481830).
In contrast to promising results with immune checkpoint inhibitors, the role of therapeutic vaccines aimed to elicit antigen-specific immune responses seems limited in patients with SCLC. The p53 protein is altered in >90% of patients with SCLC, mostly as a result of point mutations or abnormalities in degradation of wild-type p53. This leads to accumulation of mutant or wt-p53 protein and expression of p53-derived epitopes on tumor cell surfaces in the context of the MHC class I. Therefore, p53 has been suggested as a potential antigenic target to exploit with immunotherapeutic strategies (141). A clinical study conducted to assess the immunologic and clinical effects of a cancer vaccine consisting of dendritic cells (DC) transfected with a viral construct containing the full-length wild-type p53 gene (adenovirus Ad.p53) in previously treated patients with extensive stage SCLC showed low benefit in terms of clinical responses to vaccination whereas most patients had disease progression (142). However, a high rate of objective responses to chemotherapy immediately after vaccination was observed, suggesting that induction of anti-p53 cellular immunity can synergize with subsequent chemotherapy to provide potent systemic antitumor activity and that a combination strategy could be more effective. A randomized, phase II clinical trial is ongoing to evaluate this vaccine with or without all-trans retinoic acid (ATRA) after first-line standard chemotherapy treatment in extensive-stage SCLC patients (NCT00617409). It has been theorized that adding ATRA to INGN-225 will decrease the number of myeloid-derived suppressive cells and allow increased DC differentiation and function, thus improving immune responses. Objective response rate to second-line paclitaxel in each arm (with or without ATRA) is the primary objective. Preliminary results from this study have shown that administration of the vaccine after chemotherapy is safe (143). The ORR to paclitaxel was seen in 1/11, 2/12, and 3/14 patients for arms A (control), B (vaccine) and C (vaccine and ATRA), respectively. A higher positive immune response was seen in patients receiving ATRA in addition to the vaccine and this subgroup of patients also showed superior OS although survival in the vaccinated groups was inferior compared to the control group (143).
The glycosphingolipid antigen GD3 is highly expressed in SCLC but rarely expressed in normal tissues, suggesting it as a potential candidate for a vaccine. Although promising results in early studies, in a large randomized phase III trial, median OS did not differ statistically with the use of adjuvant anti-idiotypic antibody mimicking the ganglioside GD3 (Bec2/BCG) compared to best-supportive care (14.3 vs. 16.4 months, respectively; HR, 1.12; 95% CI, 0.91–1.371) in patients with limited stage SCLC (144). Other vaccines against gangliosides are being evaluated in clinical trials (NCT0134967).
MGN1703 is a novel, synthetic covalently closed DNA construct, which activates the innate immune system via the Toll-like receptor 9 (TLR9) (145,146). TLR9 is expressed on B cells and plasmacytoid dendritic cells (pDC) and recognizes bacterial and viral DNA with unmethylated cytosine-guanine dinucleotide (CpG) motifs. Once activated, pDC and B-cells upregulate co-stimulatory molecules and produce chemokines and cytokines such as interferon alpha (IFN-a), monocyte inflammatory protein 1 (MIP1), and other IFN-inducible genes to induce immune responses. MGN1703 showed immune activation and a significant stable disease rate in heavily pretreated patients with metastatic solid tumors and, at a dose of up to 60 mg twice weekly, was safe and well tolerated without dose-limiting toxicities (147). Six out of 24 patients had stable disease after six weeks of treatment; three had stable disease after a total of 12 weeks. The efficacy and safety of the immunomodulator MGN1703, a TLR9 agonist, is under investigation in a phase II trial in patients with extensive disease SCLC who achieved at least a partial response following platinum-based first-line therapy (IMPULSE study; NCT02200081).
Inhibitors of neuroendocrine markers
SCLC is a high-grade neuroendocrine tumor and some of the neuroendocrine-specific markers of this cancer could potentially be therapeutically targeted (19). The neural cell adhesion molecule 1 (NCAM1, CD56) has been identified as one of the most promising targetable markers. CD56 is expressed by tumor cells in a majority of SCLC tumor cases, as well as on cells of other tumors of neuroendocrine origin. Lorvotuzumab mertansine (BB-10901) is an antibody-drug conjugate (ADC) composed of the humanized anti-CD56 IgG1 monoclonal antibody lorvotuzumab linked to the cytotoxic, tubulin-binding maytansinoid DM1 via a disulfide linkage. A recent study demonstrated the anti-tumor activity of LM against SCLC xenograft models in mice, both as monotherapy and in combination with platinum/etoposide and paclitaxel/carboplatin, suggesting it as a promising novel effective targeted agent for SCLC therapy (148). Other studies have been completed with lorvotuzumab as monotherapy for the treatment of CD56-positive solid tumors (NCT00346385) and in combination with etoposide and carboplatin for advanced solid tumors, including extensive stage SCLC (NCT01237678).
Conclusions
SCLC is the most aggressive form of neuroendocrine tumor of the lung. No significant improvements in systemic treatments have been made in recent decades and, despite initial sensitivity of SCLC to chemotherapy and radiotherapy, patients inevitably relapse, often rapidly, and die for their disease, with a very dismal survival. A deeper characterization of the genomic landscape of SCLC has revealed that this strongly smoking-associated cancer is characterized by a very high number of somatic mutations. Genomic characterization of SCLC has been complicated by the difficulty to obtain sufficient tumor tissue to analyze since this aggressive cancer is usually diagnosed in small biopsies or cytology specimens. The advent of high-sensitive, next-generation DNA sequencing technologies has led to the identification of novel targetable molecular abnormalities. Genomic alterations have been described in classical oncogenes and tumor suppressor genes that are shared with the adenocarcinoma and squamous cell carcinoma, but also in a variety of genes involved in transcriptional regulation and chromatin modification, which seem to play a critical role in the onset and progression of this specific lung cancer tumor subtype. Gene expression governed by epigenetic changes can represent a hallmark of SCLC. Based on these new insights in SCLC biology, novel rational targeted agents have been developed and tested in clinical trials in different settings of disease. However, the majority of the trials investigating targeted therapies against specific molecules and deregulated pathways, including RTKs and specific kinases, have provided disappointing results. Furthermore, some of these trials, specifically those including anti-angiogenesis drugs, have been characterized by unacceptable toxicity. Based on these negative results, none of these targeted agents has been currently approved for clinical use for SCLC. The major limit of these studies is that most of them included patient populations not selected on the basis of the presence of specific predictive genomic alterations, thus limiting the assessment of the efficacy of these agents in these potentially high responsive subgroups of patients. Thus, there is an urgent need for predictive biomarkers to select those patients most likely to respond to treatment while sparing those potentially resistant, in order to improve the therapeutic efficacy and decrease treatment-related toxicities. Immunotherapy has recently been introduced as a new treatment option for NSCLC patients. Therapeutic vaccines in SCLC have demonstrated limited clinical efficacy. In contrast, preliminary data from clinical trials with immune checkpoint inhibitors in SCLC are promising and more robust and definitive efficacy results and correlative biomarker analyses are eagerly awaited. Finally, more preclinical studies are needed and the collection of tissue specimens from SCLC patients for tumor genotyping at baseline, and possibly at progression, is strongly advocated in order to gain new insights into this complex disease and develop novel targeted drugs and potential therapeutic combinations to improve patient outcomes. Moreover, the implementation of newer, non-invasive methods, such as liquid biopsies, in addition to next-generation sequencing techniques, will probably overcome the difficulty to obtain repeat tumor samples and allow tracking tumor genetic changes over time throughout the course of the disease.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- van Meerbeeck JP, Fennell DA, De Ruysscher DK. Small-cell lung cancer. Lancet 2011;378:1741-55. [PubMed]
- Byers LA, Rudin CM. Small cell lung cancer: where do we go from here? Cancer 2015;121:664-72. [PubMed]
- Govindan R, Page N, Morgensztern D, et al. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol 2006;24:4539-44. [PubMed]
- Kalemkerian GP, Akerley W, Bogner P, et al. Small cell lung cancer. J Natl Compr Canc Netw 2013;11:78-98. [PubMed]
- Rudin CM, Ismaila N, Hann CL, et al. Treatment of Small-Cell Lung Cancer: American Society of Clinical Oncology Endorsement of the American College of Chest Physicians Guideline. J Clin Oncol 2015;33:4106-11. [PubMed]
- O’Brien ME, Ciuleanu TE, Tsekov H, et al. Phase III trial comparing supportive care alone with supportive care with oral topotecan in patients with relapsed small-cell lung cancer. J Clin Oncol 2006;24:5441-5447. [PubMed]
- von Pawel J, Schiller JH, Shepherd FA, et al. Topotecan versus cyclophosphamide, doxorubicin, and vincristine for the treatment of recurrent small-cell lung cancer. J Clin Oncol 1999;17:658-67. [PubMed]
- Pietanza MC, Kadota K, Huberman K, et al. Phase II trial of temozolomide in patients with relapsed sensitive or refractory small cell lung cancer, with assessment of methylguanine-DNA methyltransferase as a potential biomarker. Clin Cancer Res 2012;18:1138-45. [PubMed]
- Pleasance ED, Stephens PJ, O'Meara S, et al. A small-cell lung cancer genome with complex signatures of tobacco exposure. Nature 2010;463:184-90. [PubMed]
- Takahashi T, Suzuki H, Hida T, et al. The p53 gene is very frequently mutated in small-cell lung cancer with a distinct nucleotide substitution pattern. Oncogene 1991;6:1775-8. [PubMed]
- D’Amico D, Carbone D, Mitsudomi T, et al. High frequency of somatically acquired p53 mutations in small-cell lung cancer cell lines and tumors. Oncogene 1992;7:339-46. [PubMed]
- Harbour JW, Lai SL, Whang-Peng J, et al. Abnormalities in structure and expression of the human retinoblastoma gene in SCLC. Science 1988;241:353-57. [PubMed]
- Helin K, Holm K, Niebuhr A, et al. Loss of the retinoblastoma protein-related p130 protein in small cell lung carcinoma. Proc Natl Acad Sci U S A 1997;94:6933-8. [PubMed]
- George J, Lim JS, Jang SJ, et al. Comprehensive genomic profiles of small cell lung cancer. Nature 2015;524:47-53. [PubMed]
- Peifer M, Fernandez-Cuesta L, Sos ML, et al. Integrative genome analyses identify key somatic driver mutations of small-cell lung cancer. Nat Genet 2012;44:1104-10. [PubMed]
- Rudin CM, Durinck S, Stawiski EW, et al. Comprehensive genomic analysis identifies SOX2 as a frequently amplified gene in small-cell lung cancer. Nat Genet 2012;44:1111-6. [PubMed]
- Wistuba II, Behrens C, Virmani AK, et al. High resolution chromosome 3p allelotyping of human lung cancer and preneoplastic/preinvasive bronchial epithelium reveals multiple, discontinuous sites of 3p allele loss and 3 regions of frequent breakpoints. Cancer Res 2000;60:1949-60. [PubMed]
- Bieging KT, Mello SS, Attardi LD. Unravelling mechanisms of p53-mediated tumour suppression. Nat Rev Cancer 2014;14:359-70. [PubMed]
- Semenova EA, Nagel R, Berns A. Origins, genetic landscape, and emerging therapies of small cell lung cancer. Genes Dev 2015;29:1447-62. [PubMed]
- Indovina P, Pentimalli F, Casini N, et al. RB1 dual role in proliferation and apoptosis: cell fate control and implications for cancer therapy. Oncotarget 2015;6:17873-90. [PubMed]
- Sellers WR, Novitcch BG, Miyake S, et al. Stable binding to E2F is not required for the retinoblastoma protein to activate transcription, promote differentiation, and suppress tumor cell growth. Genes Dev 1998;12:95-106. [PubMed]
- Meuwissen R, Linn SC, Linnoila RI, et al. Induction of small cell lung cancer by somatic inactivation of both Trp53 and Rb1 in a conditional mouse model. Cancer Cell 2003;4:181-9. [PubMed]
- Snitow ME, Li S, Morley MP, et al. Ezh2 represses the basal cell lineage during lung endoderm development. Development 2015;142:108-17. [PubMed]
- Coe BP, Thu KL, Aviel-Ronen S, et al. Genomic deregulation of the E2F/Rb pathway leads to activation of the oncogene EZH2 in small cell lung cancer. PLoS One 2013;8:e71670. [PubMed]
- Hubaux R, Thu KL, Coe BP, et al. EZH2 promotes E2F-driven SCLC tumorigenesis through modulation of apoptosis and cell-cycle regulation. J Thorac Oncol 2013;8:1102-6. [PubMed]
- Santarpia M, Magri I, Sanchez-Ronco M, et al. mRNA expression levels and genetic status of genes involved in the EGFR and NF-κB pathways in metastatic non-small-cell lung cancer patients. J Transl Med 2011;9:163. [PubMed]
- Bass AJ, Watanabe H, Mermel CH, et al. SOX2 is an amplified lineage-survival oncogene in lung and esophageal squamous cell carcinomas. Nat Genet 2009;41:1238-42. [PubMed]
- Pietanza MC, Ladanyi M. Bringing the genomic landscape of small-cell lung cancer into focus. Nat Genet 2012;44:1074-5. [PubMed]
- Kiefer PE, Bepler G, Kubasch M, et al. Amplification and expression of protoncogenes in human small cell lung cancer cell lines. Cancer Res 1987;47:6236-42. [PubMed]
- Hennessy BT, Smith DL, Ram PT, et al. Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat Rev Drug Discov 2005;4:988-1004. [PubMed]
- Umemura S, Mimaki S, Makinoshima H, et al. Therapeutic priority of the PI3K/AKT/mTOR pathway in small cell lung cancers as revealed by a comprehensive genomic analysis. J Thorac Oncol 2014;9:1324-31. [PubMed]
- Kraus AC, Ferber I, Bachmann SO, et al. In vitro chemo- and radio-resistance in small cell lung cancer correlates with cell adhesion and constitutive activation of AKT and MAP kinase pathways. Oncogene 2002;21:8683-95. [PubMed]
- Krystal GW, Sulanke G, Litz J. Inhibition of phosphatidylinositol 3-kinase-Akt signaling blocks growth, promotes apoptosis, and enhances sensitivity of small cell lung cancer cells to chemotherapy. Mol Cancer Ther 2002;1:913-22. [PubMed]
- Jiang SX, Sato Y, Kuwao S, et al. Expression of bcl-2 oncogene protein is prevalent in small cell lung carcinomas. J Pathol 1995;177:135-8. [PubMed]
- Ikegaki N, Katsumata M, Minna J, et al. Expression of bcl-2 in small cell lung carcinoma cells. Cancer Res 1994;54:6-8. [PubMed]
- Kaiser U, Schilli M, Haag U, et al. Expression of bcl-2-protein in small cell lung cancer. Lung Cancer 1996;15:31-40. [PubMed]
- Tanno S, Ohsaki Y, Nakanishi K, et al. Human small cell lung cancer cells express functional VEGF receptors, VEGFR-2 and VEGFR-3. Lung Cancer 2004;46:11-9. [PubMed]
- Zhan P, Wang J, Lv XJ, et al. Prognostic value of vascular endothelial growth factor expression in patients with lung cancer: a systematic review with meta-analysis. J Thorac Oncol 2009;4:1094-103. [PubMed]
- Tatematsu A, Shimizu J, Murakami Y, et al. Epidermal growth factor receptor mutations in small cell lung cancer. Clin Cancer Res 2008;14:6092-6. [PubMed]
- Pardo OE, Latigo J, Jeffery RE, et al. The fibroblast growth factor receptor inhibitor PD173074 blocks small cell lung cancer growth in vitro and in vivo. Cancer Res 2009;69:8645-51. [PubMed]
- Zhang L, Yu H, Badzio A, et al. Fibroblast Growth Factor Receptor 1 and Related Ligands in Small-Cell Lung Cancer. J Thorac Oncol 2015;10:1083-90. [PubMed]
- Rygaard K, Nakamura T, Spang-Thomsen M. Expression of the proto-oncogenes c-met and c-kit and their ligands, hepatocyte growth factor/scatter factor and stem cell factor, in SCLC cell lines and xenografts. Br J Cancer 1993;67:37-46. [PubMed]
- Rohr UP, Rehfeld N, Pflugfelder L, et al. Expression of the tyrosine kinase c-kit is an independent prognostic factor in patients with small cell lung cancer. Int J Cancer 2004;111:259-63. [PubMed]
- Badzio A, Wynes MW, Dziadziuszko R, et al. Increased insulin-like growth factor 1 receptor protein expression and gene copy number in small cell lung cancer. J Thorac Oncol 2010;5:1905-11. [PubMed]
- Maulik G, Kijima T, Ma PC, et al. Modulation of the c-Met/hepatocyte growth factor pathway in small cell lung cancer. Clin Cancer Res 2002;8:620-7. [PubMed]
- Voortman J, Harada T, Chang RP, et al. Detection and therapeutic implications of c-Met mutations in small cell lung cancer and neuroendocrine tumors. Curr Pharm Des 2013;19:833-40. [PubMed]
- Byers LA, Wang J, Nilsson MB, et al. Proteomic profiling identifies dysregulated pathways in small cell lung cancer and novel therapeutic targets including PARP1. Cancer Discov 2012;2:798-811. [PubMed]
- Ross JS, Wang K, Elkadi OR, et al. Next-generation sequencing reveals frequent consistent genomic alterations in small cell undifferentiated lung cancer. J Clin Pathol 2014;67:772-6. [PubMed]
- Park KS, Martelotto LG, Peifer M, et al. A crucial requirement for Hedgehog signaling in small cell lung cancer. Nat Med 2011;17:1504-8. [PubMed]
- Blay JY, Casali PG, Dei Tos AP, et al. Management of Gastrointestinal Stromal Tumour: Current Practices and Visions for the Future. Oncology 2015;89:1-13. [PubMed]
- Krystal GW, Honsawek S, Litz J, et al. The selective tyrosine kinase inhibitor STI571 inhibits small cell lung cancer growth. Clin Cancer Res 2000;6:3319-26. [PubMed]
- Decaudin D, de Cremoux P, Sastre X, et al. In vivo efficacy of STI571 in xenografted human small cell lung cancer alone or combined with chemotherapy. Int J Cancer 2005;113:849-56. [PubMed]
- Johnson BE, Fischer T, Fischer B, et al. Phase II study of imatinib in patients with small cell lung cancer. Clin Cancer Res 2003;9:5880-7. [PubMed]
- Krug LM, Crapanzano JP, Azzoli CG, et al. Imatinib mesylate lacks activity in small cell lung carcinoma expressing c-kit protein: a phase II clinical trial. Cancer 2005;103:2128-31. [PubMed]
- Dy GK, Miller AA, Mandrekar SJ, et al. A phase II trial of imatinib (ST1571) in patients with c-kit expressing relapsed small-cell lung cancer: a CALGB and NCCTG study. Ann Oncol 2005;16:1811-6. [PubMed]
- Schneider BJ, Kalemkerian GP, Ramnath N, et al. Phase II trial of imatinib maintenance therapy after irinotecan and cisplatin in patients with c-Kit-positive, extensive-stage small-cell lung cancer. Clin Lung Cancer 2010;11:223-7. [PubMed]
- Spigel DR, Hainsworth JD, Simons L, et al. Irinotecan, carboplatin and imatinib in untreated extensive-stage small-cell lung cancer: a phase II trial of the Minnie Pearl Cancer Research Network. J Thorac Oncol 2007;2:854-61. [PubMed]
- Boldrini L, Ursino S, Gisfredi S, et al. Expression and mutational status of c-kit in small-cell lung cancer: prognostic relevance. Clin Cancer Res 2004;10:4101-8. [PubMed]
- Lu HY, Zhang G, Cheng QY, et al. Expression and mutation of the c-kit gene and correlation with prognosis of small cell lung cancer. Oncol Lett 2012;4:89-93. [PubMed]
- Riely GJ, Yu HA. EGFR: The Paradigm of an Oncogene-Driven Lung Cancer. Clin Cancer Res 2015;21:2221-6. [PubMed]
- Moore AM, Einhorn LH, Estes D, et al. Gefitinib in patients with chemo-sensitive and chemo refractory relapsed small cell cancers: A Hoosier Oncology Group phase II trial. Lung Cancer 2006;52:93-7. [PubMed]
- Warshamana-Greene GS, Litz J, Buchdunger E, et al. The insulin-like growth factor-I receptor kinase inhibitor, NVP-ADW742, sensitizes small cell lung cancer cell lines to the effects of chemotherapy. Clin Cancer Res 2005;11:1563-71. [PubMed]
- Ferté C, Loriot Y, Clémenson C, et al. IGF-1R targeting increases the antitumor effects of DNA-damaging agents in SCLC model: an opportunity to increase the efficacy of standard therapy. Mol Cancer Ther 2013;12:1213-22. [PubMed]
- Arcaro A. Targeted therapies for small cell lung cancer: Where do we stand? Crit Rev Oncol Hematol 2015;95:154-64. [PubMed]
- Zinn RL, Gardner EE, Marchionni L, et al. ERK phosphorylation is predictive of resistance to IGF-1R inhibition in small cell lung cancer. Mol Cancer Ther 2013;12:1131-9. [PubMed]
- Schultheis AM, Bos M, Schmitz K, et al. Fibroblast growth factor receptor 1 (FGFR1) amplification is a potential therapeutic target in small-cell lung cancer. Mod Pathol 2014;27:214-21. [PubMed]
- Arriola E, Canadas I, Arumi-Uria M, et al. MET phosphorylation predicts poor outcome in small cell lung carcinoma and its inhibition blocks HGF-induced effects in MET mutant cell lines. Br J Cancer 2011;105:814-23. [PubMed]
- Rolle CE, Kanteti R, Surati M, et al. Combined MET inhibition and topoisomerase I inhibition block cell growth of small cell lung cancer. Mol Cancer Ther 2014;13:576-84. [PubMed]
- Razzini G, Berrie CP, Vignati S, et al. Novel functional PI 3-kinase antagonists inhibit cell growth and tumorigenicity in human cancer cell lines. FASEB J 2000;14:1179-87. [PubMed]
- Wojtalla A, Fischer B, Kotelevets N, et al. Targeting the phosphoinositide 3-kinase p110-α isoform impairs cell proliferation, survival, and tumor growth in small cell lung cancer. Clin Cancer Res 2013;19:96-105. [PubMed]
- Marinov M, Ziogas A, Pardo OE, et al. AKT/mTOR pathway activation and BCL-2 family proteins modulate the sensitivity of human small cell lung cancer cells to RAD001. Clin Cancer Res 2009;15:1277-87. [PubMed]
- Walls M, Baxi SM, Mehta PP, et al. Targeting small cell lung cancer harboring PIK3CA mutation with a selective oral PI3K inhibitor PF-4989216. Clin Cancer Res 2014;20:631-43. [PubMed]
- Tarhini A, Kotsakis A, Gooding W, et al. Phase II study of everolimus (RAD001) in previously treated small cell lung cancer. Clin Cancer Res 2010;16:5900-7. [PubMed]
- Sun JM, Kim JR, Do IG, et al. A phase-1b study of everolimus plus paclitaxel in patients with small-cell lung cancer. Br J Cancer 2013;109:1482-7. [PubMed]
- Besse B, Heist RS, Papadmitrakopoulou VA, et al. A phase Ib dose-escalation study of everolimus combined with cisplatin and etoposide as first-line therapy in patients with extensive-stage small-cell lung cancer. Ann Oncol 2014;25:505-11. [PubMed]
- Gardner EE, Connis N, Poirier JT, et al. Rapamycin rescues ABT-737 efficacy in small cell lung cancer. Cancer Res 2014;74:2846-56. [PubMed]
- Faber AC, Farago AF, Costa C, et al. Assessment of ABT-263 activity across a cancer cell line collection leads to a potent combination therapy for small-cell lung cancer. Proc Natl Acad Sci U S A 2015;112:E1288-96. [PubMed]
- Matsumoto M, Seike M, Noro R, et al. Control of the MYC-eIF4E axis plus mTOR inhibitor treatment in small cell lung cancer. BMC Cancer 2015;15:241. [PubMed]
- Schmid K, Bago-Horvath Z, Berger W, et al. Dual inhibition of EGFR and mTOR pathways in small cell lung cancer. Br J Cancer 2010;103:622-8. [PubMed]
- Zangemeister-Wittke U, Schenker T, Luedke GH, et al. Synergistic cytotoxicity of bcl-2 antisense oligodeoxynucleotides and etoposide, doxorubicin and cisplatin on small-cell lung cancer cell lines. Br J Cancer 1998;78:1035-42. [PubMed]
- Rudin CM, Kozloff M, Hoffman PC, et al. Phase I study of G3139, a bcl-2 antisense oligonucleotide, combined with carboplatin and etoposide in patients with small-cell lung cancer. J Clin Oncol 2004;22:1110-7. [PubMed]
- Rudin CM, Otterson GA, Mauer AM, et al. A pilot trial of G3139, a bcl-2 antisense oligonucleotide, and paclitaxel in patients with chemorefractory small-cell lung cancer. Ann Oncol 2002;13:539-45. [PubMed]
- Rudin CM., Salgia R, Wang X, et al. Randomized phase II study of carboplatin and etoposide with or without the bcl-2 antisense oligonucleotide oblimersen for extensive-stage small-cell lung cancer: CALGB 30103. J Clin Oncol 2008;26:870-6. [PubMed]
- Li J, Viallet J, Haura E. A small molecule pan-Bcl-2 family inhibitor, GX15-070, induces apoptosis and enhances cisplatin-induced apoptosis in non-small cell lung cancer cells. Cancer Chemother Pharmacol 2008;61:525-34. [PubMed]
- Paik PK, Rudin CM, Brown A, et al. A phase I study of obatoclax mesylate, a Bcl-2 antagonist, plus topotecan in solid tumor malignancies. Cancer Chemother Pharmacol 2010;66:1079-85. [PubMed]
- Langer CJ, Albert I, Ross HJ, et al. Randomized phase II study of carboplatin and etoposide with or without obatoclax mesylate in extensive-stage small cell lung cancer. Lung Cancer 2014;85:420-8. [PubMed]
- Paik PK, Rudin CM, Pietanza MC, et al. A phase II study of obatoclax mesylate, a Bcl-2 antagonist, plus topotecan in relapsed small cell lung cancer. Lung Cancer 2011;74:481-5. [PubMed]
- Gandhi L, Camidge DR, Ribeiro de Oliveira M, et al. Phase I study of Navitoclax (ABT-263), a novel Bcl-2 family inhibitor, in patients with small-cell lung cancer and other solid tumors. J Clin Oncol 2011;29:909-16. [PubMed]
- Rudin CM, Hann CL, Garon EB, et al. Phase II study of single-agent navitoclax (ABT-263) and biomarker correlates in patients with relapsed small cell lung cancer. Clin Cancer Res 2012;18:3163-9. [PubMed]
- Watkins DN, Berman DM, Burkholder SG, et al. Hedgehog signalling within airway epithelial progenitors and in small-cell lung cancer. Nature 2003;422:313-7. [PubMed]
- Belani CP, Dahlberg SE, Rudin CM, et al. Three-arm randomized phase II study of cisplatin and etoposide (CE) versus CE with either vismodegib (V) or cixutumumab (Cx) for patients with extensive stage-small cell lung cancer (ES-SCLC) (ECOG 1508). J Clin Oncol 2013;31:abstr 7508.
- Abbotts R, Thompson N, Madhusudan S. DNA repair in cancer: emerging targets for personalized therapy. Cancer Manag Res 2014;6:77-92. [PubMed]
- Simbulan-Rosenthal CM, Rosenthal DS, Luo R, et al. PARP-1 binds E2F-1 independently of its DNA binding and catalytic domains, and acts as a novel coactivator of E2F-1-mediated transcription during re-entry of quiescent cells into S phase. Oncogene 2003;22:8460-71. [PubMed]
- Calabrese CR, Almassy R, Barton S, et al. Anticancerchemosensitization and radiosensitization by the novel poly(ADP-ribose) polymerase-1 inhibitor AG14361. J Natl Cancer Inst 2004;96:56-67. [PubMed]
- Farmer H. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 2005;434:917-21. [PubMed]
- Cardnell RJ, Feng Y, Diao L, et al. Proteomic markers of DNA repair and PI3K pathway activation predict response to the PARP inhibitor BMN 673 in small cell lung cancer. Clin Cancer Res 2013;19:6322-8. [PubMed]
- Wainberg ZA, Rafii S, Ramanathan RK, et al. Safety and antitumor activity of the PARP inhibitor BMN673 in a phase I trial recruiting metastatic small-cell lung cancer (SCLC) and germline BRCA-mutation carrier cancer patients. J Clin Oncol 2014;32:abstr 7522.
- Owonikoko TK, Dahlberg SE, Khan SA, et al. A phase I safety study of veliparib combined with cisplatin and etoposide in extensive stage small cell lung cancer: A trial of the ECOG-ACRIN Cancer Research Group (E2511). Lung Cancer 2015;89:66-70. [PubMed]
- Delmore JE, Issa GC, Lemieux ME, et al. BET bromodomain inhibition as a therapeutic strategy to target c-Myc. Cell 2011;146:904-17. [PubMed]
- Mertz JA, Conery AR, Bryant BM, et al. Targeting MYC dependence in cancer by inhibiting BET bromodomains. Proc Natl Acad Sci U S A 2011;108:16669-74. [PubMed]
- Christensen CL, Kwiatkowski N, Abraham BJ, et al. Targeting transcriptional addictions in small cell lung cancer with a covalent CDK7 inhibitor. Cancer Cell 2014;26:909-22. [PubMed]
- Hilton JF, Shapiro GI. Aurora kinase inhibition as an anticancer strategy. J Clin Oncol 2014;32:57-9. [PubMed]
- Sos ML, Dietlein F, Peifer M, et al. A framework for identification of actionable cancer genome dependencies in small cell lung cancer. Proc Natl Acad Sci U S A 2012;109:17034-9. [PubMed]
- Hook KE, Garza SJ, Lira ME, et al. An integrated genomic approach to identify predictive biomarkers of response to the aurora kinase inhibitor PF-03814735. Mol Cancer Ther 2012;11:710-9. [PubMed]
- Melichar B, Adenis A, Lockhart AC, et al. Safety and activity of alisertib, an investigational aurora kinase A inhibitor, in patients with breast cancer, small-cell lung cancer, non-small-cell lung cancer, head and neck squamous-cell carcinoma, and gastro-oesophageal adenocarcinoma: a five-arm phase II study. Lancet Oncol 2015;16:395-405. [PubMed]
- Bolden JE, Peart MJ, Johnstone RW. Anticancer activities of histone deacetylase inhibitors. Nat Rev Drug Discov 2006;5:769-84. [PubMed]
- Tsurutani J, Soda H, Oka M, et al. Antiproliferative effects of the histone deacetylase inhibitor FR901228 on small-cell lung cancer lines and drug-resistant sublines. Int J Cancer 2003;104:238-42. [PubMed]
- Crisanti MC, Wallace AF, Kapoor V, et al. The HDAC inhibitor panobinostat (LBH589) inhibits mesothelioma and lung cancer cells in vitro and in vivo with particular efficacy for small cell lung cancer. Mol Cancer Ther 2009;8:2221-31. [PubMed]
- Hubaux R, Vandermeers F, Crisanti MC, et al. Preclinical evidence for a beneficial impact of valproate on the response of small cell lung cancer to first-line chemotherapy. Eur J Cancer 2010;46:1724-34. [PubMed]
- Luszczek W, Cheriyath V, Mekhail TM, et al. Combinations of DNA methyltransferase and histone deacetylase inhibitors induce DNA damage in small cell lung cancer cells: correlation of resistance with IFN-stimulated gene expression. Mol Cancer Ther 2010;9:2309-21. [PubMed]
- de Marinis F, Atmaca A, Tiseo M, et al. A phase II study of the histone deacetylase inhibitor panobinostat (LBH589) in pretreated patients with small-cell lung cancer. J Thorac Oncol 2013;8:1091-4. [PubMed]
- Trepel J, Mollapour M, Giaccone G, et al. Targeting the dynamic HSP90 complex in cancer. Nat Rev Cancer 2010;10:537-49. [PubMed]
- Lai CH, Park KS, Lee DH, et al. HSP-90 inhibitor ganetespib is synergistic with doxorubicin in small cell lung cancer. Oncogene 2014;33:4867-76. [PubMed]
- Ready NE, Dudek AZ, Pang HH, et al. Cisplatin, irinotecan, and bevacizumab for untreated extensive-stage small-cell lung cancer: CALGB 30306, a phase II study. J Clin Oncol 2011;29:4436-41. [PubMed]
- Horn L, Dahlberg SE, Sandler AB, et al. Phase II study of cisplatin plus etoposide and bevacizumab for previously untreated, extensive-stage small-cell lung cancer: Eastern Cooperative Oncology Group Study E3501. J Clin Oncol 2009;27:6006-11. [PubMed]
- Spigel DR, Greco FA, Zubkus JD, et al. Phase II trial of irinotecan, carboplatin, and bevacizumab in the treatment of patients with extensive-stage small-cell lung cancer. J Thorac Oncol 2009;4:1555-60. [PubMed]
- Spigel DR, Townley PM, Waterhouse DM, et al. Randomized phase II study of bevacizumab in combination with chemotherapy in previously untreated extensive-stage small-cell lung cancer: results from the SALUTE trial. J Clin Oncol 2011;29:2215-22. [PubMed]
- Tiseo M, Boni L, Ambrosio F, et al. Italian multicenter phase III randomized study of cisplatin-etoposide with or without bevacizumab as first-line treatment in extensive stage small cell lung cancer: treatment rationale and protocol design of the GOIRC-AIFA FARM6PMFJM trial. Clin Lung Cancer 2015;16:67-70. [PubMed]
- Mountzios G, Emmanouilidis C, Vardakis N, et al. Paclitaxel plus bevacizumab in patients with chemoresistant relapsed small cell lung cancer as salvage treatment: a phase II multicenter study of the Hellenic Oncology Research Group. Lung Cancer 2012;77:146-50. [PubMed]
- Spigel DR, Waterhouse DM, Lane S, et al. Efficacy and safety of oral topotecan and bevacizumab combination as second-line treatment for relapsed small-cell lung cancer: an open-label multicenter single-arm phase II study. Clin Lung Cancer 2013;14:356-63. [PubMed]
- Gitlitz BJ, Moon J, Glisson BS, et al. Sorafenib in platinum-treated patients with extensive stage small cell lung cancer: a Southwest Oncology Group (SWOG 0435) phase II trial. J Thorac Oncol 2010;5:1835-40. [PubMed]
- Sharma N, Pennell N, Nickolich M, et al. Phase II trial of sorafenib in conjunction with chemotherapy and as maintenance therapy in extensive-stage small cell lung cancer. Invest New Drugs 2014;32:362-8. [PubMed]
- Ready N, Dunphy F, Pang H, et al. Combination chemotherapy with sunitinib (IND 74019; NSC 736511) for untrated extensive-stage small cell lung cancer (SCLC): CALGB 30504 phase IB safety results. J Clin Oncol 2010;28:abstr 7056.
- Han JY, Kim HY, Lim KY, et al. A phase II study of sunitinib in patients with relapsed or refractory small cell lung cancer. Lung Cancer 2013;79:137-42. [PubMed]
- Schneider BJ, Gadgeel SM, Ramnath N, et al. Phase II trial of sunitinib maintenance therapy after platinum-based chemotherapy in patients with extensive-stage small cell lung cancer. J Thorac Oncol 2011;6:1117-20. [PubMed]
- Spigel DR, Greco FA, Rubin MS, et al. Phase II study of maintenance sunitinib following irinotecan and carboplatin as first-line treatment for patients with extensive-stage small-cell lung cancer. Lung Cancer 2012;77:359-64. [PubMed]
- Ready NE, Pang HH, Gu L, et al. Chemotherapy With or Without Maintenance Sunitinib for Untreated Extensive-Stage Small-Cell Lung Cancer: A Randomized, Double-Blind, Placebo Controlled Phase II Study-CALGB 30504 (Alliance). J Clin Oncol 2015;33:1660-5. [PubMed]
- Ramalingam SS, Belani CP, Mack PC, et al. Phase II study of cediranib (AZD 2171), an inhibitor of the vascular endothelial growth factor receptor, for second- line therapy of small cell lung cancer (National Cancer Institute #7097). J Thorac Oncol 2010;5:1279-84. [PubMed]
- Arnold AM, Seymour L, Smylie M, et al. Phase II study of vandetanib or placebo in small-cell lung cancer patients after complete or partial response to induction chemotherapy with or without radiation therapy. National Cancer Institute of Canada Clinical Trials Group Study BR.20. J Clin Oncol 2007;25:4278-84. [PubMed]
- Lee SM, Woll PJ, Rudd R, et al. Anti-angiogenic therapy using thalidomide combined with chemotherapy in small cell lung cancer: a randomized, double-blind, placebo-controlled trial. J Natl Cancer Inst 2009;101:1049-57. [PubMed]
- Pujol JL, Breton JL, Gervais R, et al. Phase III double-blind, placebo-controlled study of thalidomide in extensive-disease small-cell lung cancer after response to chemotherapy: an intergroup study FNCLCC cleo04 IFCT 00-01. J Clin Oncol 2007;25:3945-51. [PubMed]
- Allen JW, Moon J, Redman M, et al. Southwest Oncology Group S0802: a randomized, phase II trial of weekly topotecan with and without ziv-aflibercept in patients with platinum-treated small-cell lung cancer. J Clin Oncol 2014;32:2463-70. [PubMed]
- Viganò MG, Cavina R, Novello S, et al. Phase II trial of NGR-hTNF and doxorubicin in relapsed small cell lung cancer (SCLC). J Clin Oncol 2011;29:abstr 7077.
- Lawrence MS, Stojanov P, Polak P, et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 2013;499:214-8. [PubMed]
- Bustamante Alvarez JG, González-Cao M, Karachaliou N, et al. Advances in immunotherapy for treatment of lung cancer. Cancer Biol Med 2015;12:209-22. [PubMed]
- Santarpia M, Karachaliou N. Tumor immune microenvironment characterization and response to anti-PD-1 therapy. Cancer Biol Med 2015;12:74-8. [PubMed]
- Santarpia M, González-Cao M, Viteri S, et al. Programmed cell death protein-1/programmed cell death ligand-1 pathway inhibition and predictive biomarkers: understanding transforming growth factor-beta role. Transl Lung Cancer Res 2015;4:728-42. [PubMed]
- Ishii H, Azuma K, Kawahara A, et al. Significance of programmed cell death-ligand 1 expression and its association with survival in patients with small cell lung cancer. J Thorac Oncol 2015;10:426-30. [PubMed]
- Reck M, Bondarenko I, Luft A, et al. Ipilimumab in combination with paclitaxel and carboplatin as first-line therapy in extensive-disease-small-cell lung cancer: results from a randomized, double-blind, multicenter phase II trial. Ann Oncol 2013;24:75-83. [PubMed]
- Ott PA, Fernandez MEE, Hiret S, et al. Pembrolizumab (MK-3475) in patients (pts) with extensive-stage small cell lung cancer (SCLC): Preliminary safety and efficacy results from KEYNOTE-028. J Clin Oncol 2015;33:abstr 7502.
- Freeman-Keller M, Goldman J, Gray J. Vaccine immunotherapy in lung cancer: Clinical experience and future directions. Pharmacol Ther 2015;153:1-9. [PubMed]
- Antonia SJ, Mirza N, Fricke I, et al. Combination of p53 cancer vaccine with chemotherapy in patients with extensive stage small cell lung cancer. Clin Cancer Res 2006;12:878-87. [PubMed]
- Chiappori A, Antonia S, Williams, C, et al. P53 dendritic cell vaccine in small cell lung cancer. Journal of Thoracic Oncology 2014;9:abstr P1.30.
- Giaccone G, Debruyne C, Felip E, et al. Phase III study of adjuvant vaccination with Bec2/bacille Calmette-Guerin in responding patients with limited-disease small-cell lung cancer (European Organisation for Research and Treatment of Cancer 08971-08971B; Silva Study). J Clin Oncol 2005;23:6854-64. [PubMed]
- Kanzler H, Barrat FJ, Hessel EM, et al. Therapeutic targeting of innate immunity with Toll-like receptor agonists and antagonists. Nat Med 2007;13:552-9. [PubMed]
- Krieg AM. Therapeutic potential of Toll-like receptor 9 activation. Nat Rev Drug Discov 2006;5:471-84. [PubMed]
- Weihrauch MR, Richly H, von Bergwelt-Baildon MS, et al. Phase I clinical study of the toll-like receptor 9 agonist MGN1703 in patients with metastatic solid tumours. Eur J Cancer 2015;51:146-56. [PubMed]
- Whiteman KR, Johnson HA, Mayo MF, et al. Lorvotuzumab mertansine, a CD56-targeting antibody-drug conjugate with potent antitumor activity against small cell lung cancer in human xenograft models. MAbs 2014;6:556-66. [PubMed]


