
The improved success rate and reduced complications of a novel localization device vs. hookwire for thoracoscopic resection of small pulmonary nodules: a single-center, open-label, randomized clinical trial
Introduction
With the widespread application of high-resolution low-dose computed tomography (CT) for lung cancer screening, the detection of small pulmonary nodules with suspicious malignancy at a very early stage has increased (1), leading to a considerable number of patients undergoing surgery. However, the detected pulmonary nodules present a significant surgical challenge in that their small size makes them difficult to visualize or palpate during video-assisted thoracoscopic surgery (VATS), particularly when the location is distant from the visceral pleura. This challenge can result in a conversion thoracotomy rate of up to 46% (2) or even unnecessary lobectomy.
Currently, many different localization techniques have been applied in clinics to facilitate the successful resection of pulmonary nodules, including hookwire under the guidance of preoperative CT, microcoil, methylene blue, or lipiodol fiducial marker (3-7). Among these, the hookwire is the most widely-used device for the preoperative localization of pulmonary nodules owing to its reliable successful localization rate (80.6–99.6%), short localization duration, and low cost (8-10). However, it is associated with a relatively high rate of complications, such as chest pain, pneumothorax (7.5–56.2%), dislodgement (0.4–19.4%), lung parenchyma hemorrhage (10.3–25.8%), subcutaneous emphysema (5%), hemothorax (1.1%), vasovagal syncope (0.6%), and systemic air embolism (0.2–0.6%) (1,8,9,11-18). To resolve these limitations of hookwire or other similar devices, we developed a new device that has a 4-hook anchor with scaled suture, which demonstrated a high localization success rate, good patient tolerance, and a low rate of complications in the preoperative localization of pulmonary nodules in a multi-center single-arm clinical trial (19).
Here, we conducted a single-center, open-label, prospective, randomized clinical trial to compare the effectiveness, safety, and patient tolerance between our novel localization device and the hookwire for the preoperative localization of pulmonary nodules. We present the following article in accordance with the CONSORT reporting checklist (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-555/rc) (20).
Methods
Study design and participants
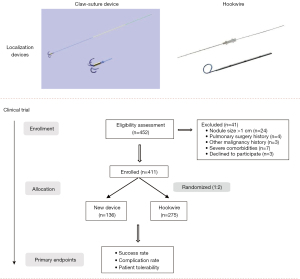
This prospective, single-center, randomized clinical trial was performed in accordance with the Declaration of Helsinki (as revised in 2013). The study design and flow diagram are shown in Figure 1. Patients who received CT-guided localization procedures at Shanghai Chest Hospital from October to December 2020 were assessed for enrollment. A consent form was signed by each patient approving participation in this trial as well as the use of their clinical data. This study was approved by the Ethics Committee of Shanghai Chest Hospital (No. KS1972).
Patients aged 18–80 years old who had small pulmonary nodules (diameter 0.4–1 cm) and had planned to undergo localization and VATS were enrolled. Those with a performance status <3 and without a significantly enlarged lung hilus or mediastinal lymph node on CT examination were included. The exclusion criteria were as follows: (I) patients with sepsis, repeated pulmonary infection, or any type of severe infectious diseases 30 days before surgery; (II) patients with severe heart, brain, lung, liver, or kidney comorbidities, or severe hypertension; (III) patients with severe coagulation disorders; (IV) patients with any advanced diseases or distant metastasis; and (V) patients who had participated in other clinical trials within 30 days before screening.
All CT-guided localizations of pulmonary nodules were performed by two radiologists who had more than 5 years of experience in CT-guided intervention. After localization, patients underwent resection for pulmonary nodules. The localization device was removed from the pulmonary tissue during the surgery as the lesion was resected. Cases that did not complete the localization process and VATS were excluded.
Randomization
Owing to the large volume of our center, more patients were enrolled based on the trial protocol by surgeons. The patients were randomly assigned (1:2 ratio) into either the claw group and the hookwire group via computer-generated randomized numbers [using Stata 14 software (StataCorp, College Station, TX, USA)] by the laboratory investigators, and both the surgeons, the radiologists, and the patients were masked as to the allocation schedule. Sealed and numbered envelopes that contained the allocated group for each patient were prepared and opened at the beginning of each localization procedure. Since the novel device has not been verified by large sample clinical trials, and hookwire is the most widely used device in our center, more enrolled patients are assigned to the hookwire group.
Sample size
The sample size was calculated using PASS 11 software (NCSS, Kaysville, UT, USA) and Fisher’s exact test. According to some references and our previous study (8-10,19), we considered the success rate of hookwire as 89%, and p2 represented the success rate of the novel localization device (97%), with one-sided test and the 1:2 ratio of the control and intervention groups. To achieve a statistical power (1 − β) of 80% and a type I error (α) of 5%, 116 patients were needed in the control group and 232 patients in the intervention group. Assuming an approximate 15% drop-out rate, we needed to enroll at least 136 patients in the control group and 273 in the intervention group.
CT-guided localization
This novel claw-suture localization device was designed and manufactured by us and a biotechnology company (Senscure, Ningbo, China), and the details were introduced in our previous study (19). Briefly, it consists of six parts: coaxial needle, pusher, anchor claw, suture, release buckle, and protection tube. The main features of this device are an anchor claw with four blunt-ended hooks and an absorbable tri-colored suture (Figure 1); the former increases the reliability of localization, while the latter contributes to exposure and assists surgeons in intraoperatively evaluating the depth of localization. The hookwire is the most commonly used device for pulmonary nodule localization in our center and its application has been reported by numerous studies (9,21). The novel claw-suture device is used in a similar manner to the hookwire during localization.
The process of localization was as follows (Figure 2): (I) the patient was placed in an appropriate position on the CT table based on the location of the pulmonary nodule, and then a non-enhanced CT scan was performed to determine the location of the nodule; (II) according to the position of the nodule and the distance between the nodule and the skin on the CT image, the optimal puncture site, angle, and route for introducer needle insertion were determined; (III) after local anesthesia of the puncture site, the coaxial needle was gradually inserted into the chest wall (Figure 2A); (IV) CT scan was performed again to verify whether the needle was in the right direction, and then the tip of the needle was inserted to the measured distance; (V) CT scan was performed to confirm that the needle was in the ideal position (the needle tip was as close as possible to the lesion) (Figure 2B); (VI) the hookwire or the claw-suture system was released, the coaxial needle was removed, and a further CT scan was subsequently performed to confirm the exact location of the marker and the absence of immediate complications such as pneumothorax or parenchymal bleeding (Figure 2C); and (VII) after checking the patient’s vital signs and complaints, they were transported to the operating room for thoracoscopic resection (Figure 2D-2F). After localization, a discussion between surgeons and radiologists confirmed the relative position of the nodule and marker.
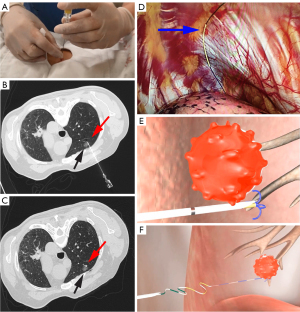
Surgical procedure
All of the enrolled patients received VATS wedge resection or segmentectomy after successful localization. During the first exploration by VATS, surgeons found the localization marker, checked the integrity, and tried to determine the position of the lesion by finger palpation and CT imaging (Figure 2D). All of the lesions were sent for intraoperative frozen pathological examinations, and segmentectomy or lobectomy was performed if necessary. All of the targeted nodules were successfully resected on the first attempt, which was confirmed by frozen sectioning. Negative surgical margins were confirmed for all sublobar resections.
Evaluation
The clinical data, localization characteristics, complications, and degree of pain were evaluated. The primary endpoint was the localization success rate of the claw-suture device and hookwire for single and multiple nodules. The secondary endpoints included the complication rate, localization-related time, and degree of pain. Both the primary and secondary endpoints were evaluated during the entire procedure until the completion of the surgery. The success of localization was measured as follows: (I) the anchor claw was placed around the nodule (within 10 mm); (II) during the procedure, the equipment was placed and retrieved smoothly, and no faults occurred; (III) there was no dislodgement of the device from the localization procedure to the first VATS exploration. Additionally, the dislodgement was identified as the localizer moving from the original place or out of the lung parenchyma, which was found at the time of the first thoracoscopy exploration. The pain visual analog scale [0–10] was used to quantify the pain intensity after localization (22). Pain alleviation was defined as the difference between the two visual analog scale scores measured immediately after localization and 10 min later. Whether body movement increased chest pain was also recorded. No follow-up was required.
Statistical analyses
All the enrolled patients were included in analysis (intention-to-treat). The quantitative data were expressed by the average, standard deviation (SD), and range, Categorical variables were described as numbers and percentages. The two-sided Student’s t-test was used to test differences between continuous variables, and the Chi-square test or Fisher’s exact test (if expected frequency <5) was applied for categorical variables. Risk difference and risk ratio were used as effect size to describe the difference of ratio. A P value less than 0.05 was considered statistically significant (two-sided). All statistical analyses were conducted using SPSS 22 software (IBM Corporation, Chicago, IL, USA). Subgroup analysis was performed in patients who received multiple localizations.
Results
Patients’ characteristics
From October to December 2020, a total of 411 patients [130 men, 281 women, mean age of 53.7±12.6 (range, 18–80) years] who received pulmonary nodules localization and VATS were included in the final analysis. Another 41 patients who did not meet the inclusion criteria or refused to sign the consent form were excluded. 136 patients underwent localization using the claw-suture system (claw group) and 275 patients using the hookwire (hookwire group) (Figure 1). The patients’ characteristics are shown in Table 1. The sizes of localized pulmonary nodules (0.71±0.15 vs. 0.70±0.14 cm, P=0.594) were not significantly different between the two groups, neither were the other baseline data.
Table 1
| Variables | Claw group (n=136) | Hookwire group (n=275) | P value |
|---|---|---|---|
| Gender, n (%) | 0.819 | ||
| Male | 42 (30.9) | 88 (32.0) | |
| Female | 94 (69.1) | 187 (68.0) | |
| Age (years), mean ± SD, range | 52.0±11.2, 18–80 | 54.5±13.2, 18–80 | 0.053 |
| Lesion size (diameter, cm), mean ± SD, range | 0.71±0.15, 0.4–1.0 | 0.70±0.14, 0.4–1.0 | 0.594 |
| Lesion location, n (%) | 0.469 | ||
| Right | 75 (55.1) | 148 (53.8) | |
| Left | 61 (44.9) | 124 (45.1) | |
| Bilateral | 0 (0.0) | 3 (1.1) | |
| Localized lesion number, n (%) | 0.140 | ||
| Single | 103 (75.7) | 189 (68.7) | |
| Two or more | 33 (24.3) | 86 (31.3) | |
| Localization time (min), mean ± SD, range | 14.4±6.6, 5–36 | 7.2±2.9, 4–20 | <0.001* |
| Localization results, n (%) | 0.027* | ||
| Success | 133 (97.8) | 254 (92.4) | |
| Failure | 3 (2.2) | 21 (7.6) | |
| Pneumothorax, n (%) | 0.397 | ||
| Yes | 37 (27.2) | 86 (31.3) | |
| No | 99 (72.8) | 189 (68.7) | |
| Hemorrhage, n (%) | 0.003* | ||
| Yes | 23 (16.9) | 103 (37.5) | |
| No | 113 (83.1) | 172 (62.5) | |
| Pleural reaction, n (%) | 0.017* | ||
| Yes | 0 (0.0) | 14 (5.1) | |
| No | 136 (100.0) | 261 (94.9) | |
| Pain visual analog scale, mean ± SD, range | |||
| After localization | 2.4±1.8, 0–7 | 2.4±2.1, 0–9 | 0.973 |
| 10 min after localization | 1.4±1.9, 0–7 | 2.0±1.9, 0–8 | 0.087 |
| Pain alleviation | 0.84±0.98, −1 to 4 | 0.35±0.79, −2 to 4 | <0.001* |
*, statistically significant. SD, standard deviation.
Procedure results
Thirty-three cases (24.3%) in the claw group and 86 cases (31.3%) in the hookwire group had two or more lesions localized, respectively. No device faults occurred during any of the procedures, and all devices were retrieved from the resected specimens. The success rate in the claw group was significantly higher than that in the hookwire group (97.8% vs. 92.4%, P=0.027; risk ratio =1.058, risk difference =0.054) (Table 1). Moreover, among the patients who received multiple localizations, the claw group had a higher success rate than the hookwire group (97.0% vs. 81.4%, P=0.038; risk ratio =1.192, risk difference =0.156) (Table 2). The details are shown in Table 3. The mean localization time in the hookwire group was significantly shorter than that in the claw group (7.2±2.9 vs. 14.4±6.6 min, P<0.001).
Table 2
| Variables | Claw group (n=33) | Hookwire group (n=86) | P value |
|---|---|---|---|
| Localization time (min), mean ± SD, range | 14.7±5.8, 6–25 | 10.2±3.0, 5–20 | <0.001* |
| Localization results, n (%) | 0.038* | ||
| Success | 32 (97.0) | 70 (81.4) | |
| Failure | 1 (3.0) | 16 (18.6) | |
| Pneumothorax, n (%) | 0.433 | ||
| Yes | 18 (54.5) | 40 (46.5) | |
| No | 15 (45.5) | 46 (53.5) | |
| Hemorrhage, n (%) | 0.128 | ||
| Yes | 11 (33.3) | 42 (48.8) | |
| No | 22 (66.7) | 44 (51.2) | |
| Pleural reaction, n (%) | 0.032* | ||
| Yes | 0 (0.0) | 14 (16.3) | |
| No | 33 (100.0) | 72 (83.7) | |
| Pain visual analog scale, mean ± SD, range | |||
| After localization | 3.0±1.7, 0–7 | 3.3±2.4, 0–9 | 0.456 |
| 10 min after localization | 2.3±2.0, 0–7 | 2.8±2.4, 0–8 | 0.450 |
| Pain alleviation | 0.83±1.1, 0–4 | 0.37±0.81, −2 to 3 | 0.056 |
*, statistically significant. SD, standard deviation.
Table 3
| Number of localized nodules | Localization results, success/failure (%) | P value | |
|---|---|---|---|
| Claw group (n=33) | Hookwire group (n=86) | ||
| 2 | 21/0 (100.0) | 49/3 (94.2) | 0.552 |
| 3 | 10/0 (100.0) | 18/7 (72.0) | 0.084 |
| 4 | 1/1 (50.0) | 3/4 (42.9) | |
| 5 | 0/0 (0.0) | 0/2 (0.0) | |
Unsuccessful cases
There were three cases of dislodgement in the claw group, two of which were due to the lesion being so shallow to the surface of the visceral pleural that the coaxial needle did not break through it, and one case was caused by improper operation.
As for the 21 unsuccessful cases in the hookwire group, there were 12 cases of the hookwires moving from the original place but were still in the lung parenchyma, eight cases of the hookwires being found in the pleural cavity, and one case of the hookwire completely retreating into the chest wall.
Complications
Overall, no deaths or other severe adverse events occurred during the study procedures. The rate of hemorrhage in the claw group was markedly lower than that in the hookwire group (16.9% vs. 37.5%, P=0.003; risk ratio =0.451, risk difference =−0.206). No significant difference was observed in the rate of pneumothorax between the two groups (27.2% vs. 31.3%, P=0.397). Notably, pleural reaction requiring medical intervention was observed in 14 cases in the hookwire group, while no pleural reaction was observed in the claw group (5.1% vs. 0%, P=0.017; risk ratio =0.072, risk difference =−0.047) (Table 1). No symptomatic complications requiring medical intervention were observed in the claw group. Although the patients’ pain scores immediately after localization (2.4±1.8 vs. 2.4±2.1, P=0.973) and 10 min later (1.4±1.9 vs. 2.0±1.9, P=0.087) were not significantly different between the two groups, pain alleviation in the claw group was substantially better than that in the hookwire group 10 min after localization (0.84±0.98 vs. 0.35±0.79, P<0.001). All patients in the claw group stated that their body movement did not increase their chest pain while they waited for the VATS procedure.
As for patients who received multiple localizations, there was a significantly higher incidence of pleural reaction in the hookwire group (16.3% vs. 0%, P=0.032; risk ratio =0.093, risk difference =−0.148). No significant differences in the incidence of pneumothorax (54.5% vs. 46.5%) and hemorrhage (33.3% vs. 48.8%) were observed between the two groups (Table 2).
Discussion
Our study showed that the claw-suture device for localization was as safe and feasible as hookwire for preoperative pulmonary nodule localization, and could be used for diagnosis and treatment. Consistent with our previous multi-center study, this device is well-tolerated by patients and easily placed by radiologists, causes few complications, and fixes reliably in the lung parenchyma (19).
From the above, we considered that this novel device has some advantages over hookwire for the localization of small pulmonary nodules. The anchor claw has four fishhook-shaped blunt tips. When the claw is released, it completely “inserts” into the adjacent lung tissue. The release process of the claw is gradually and gently extended, making the fixation more reliable and less invasive. The data from this study showed a significant improvement in the success rates of the claw-suture device compared to the hookwire. Next, unlike the long, hard hookwire, the soft and flexible suture can be pushed into the thorax upon completion of the localization process, which effectively avoids the tension force of the chest wall to the anchor claw, thereby reducing the rate of dislodgement. At the same time, the suture is well tolerated by patients and does not limit their body activity compared with the metal tail of the hookwire, which was confirmed by other researchers who also replaced the metal wire with a suture (12,14,15,23,24). Our data also demonstrated that patients in the claw group felt less pain than those in the hookwire group. Notably, it is important that no pleural reaction, which causes patient discomfort and even leads to shock or syncope, occurred in the claw group (25). Seo et al. (17) reported that vasovagal syncope was observed at a rate of 0.6% in lung nodule localizations using a hookwire. So, patients receiving localization using a hookwire need to be positioned and transferred carefully.
During surgery, the suture can be pulled up to lift the adjacent lung tissue, creating a better exposure of the operative field and making the procedure more convenient. Additionally, the suture is equally divided into three parts with different colors so that surgeons can know how deep the claw is beneath the surface of the visceral pleural. As a result, this device can increase the localization depth while ensuring safety during wedge resections. As for the hookwire, it cannot withstand pulling because it has only one hook, and its long metal tail can interfere with the surgeon’s operation, which needs to be cut short, making it easier to be lost or left in the chest (26). Moreover, even though the localization depth could be measured by CT scan before the operation, it is difficult to accurately determine the depth of the wire intraoperatively due to the absence of scale on the wire and lung collapse. Hence, the hookwire is likely to be cut off using a stapler during sublobectomy and retained in the lung. Both Miyoshi et al. and Iguchi et al. (14,26) reported cases in which the hookwires were not recovered from the resected specimens and left in the lung, with an incidence rate of 2.4% and 0.4%, respectively.
In addition to the success rate, safety and complication rate are important concerns in pulmonary nodule localization. The results of this study showed that both the claw and hookwire caused no major complications. A slightly lower (not significant) incidence of pneumothorax was observed in the claw group compared to the hookwire group, which might have been caused by the puncture of the coaxial needle instead of the claw. In our center, the hookwire has been the most commonly used device used for pulmonary nodule localization for more than 5 years, while the new claw-suture system has only been formally used (infrequently) for less than 2 years. Therefore, the inexperience of the radiologists with the new system might increase the complication rate. However, Yi et al. and other researchers (12,18,27) reported major complications with the hookwire, such as systemic air embolism. Furthermore, the hookwire was originally invented for breast nodule localization, so it might not be the ideal choice for pulmonary nodules.
The main limitations of our study are the limited sample size and the single-center design. Importantly, cases in which the nodule was close to the visceral pleura need to be dealt with care. The distal end of the coaxial needle should be introduced a little further beyond the lesion in case it did not break through the visceral pleura. Further large-sample multi-center randomized clinical trials are warranted to confirm the safety and effectiveness of this device.
In conclusion, this new claw-suture system is a safe, feasible, and well-tolerated method for the localization of small pulmonary nodules, which could be an option to replace the hookwire. Following the localization procedure, the degree of pain among patients was limited and their activity was not restricted.
Acknowledgments
The authors appreciate the academic support from AME Thoracic Surgery Collaborative Group. The authors also appreciate the great support from Dr. Gorka Bastarrika (University of Navarra School of Medicine, Spain) for improving the quality of this paper.
Funding: This research was supported by the Multidisciplinary Collaborative Innovation Project of Shanghai Chest Hospital and the Science and Technology Development Project of Shanghai Municipality (No. 19411963900 to FY) and the Medical-Engineering Interdisciplinary Research project of Shanghai Jiao Tong University (No. YG2021QN128 to ZW).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-555/rc
Trial Protocol: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-555/tp
Data Sharing Statement: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-555/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-555/coif). ZW reports that this research was supported by the Medical-Engineering Interdisciplinary Research project of Shanghai Jiao Tong University (No. YG2021QN128 to ZW). JCS received Noah’s Hope and Hope 4 Bridget Grant, payment for expert testimony from NIH study section. JCS has a family member that is a shareholder and receives compensation from VIDA Diagnostics, a company commercializing lung image analysis software. This software was not used for this publication. FY reports that this research was funded by the Multidisciplinary Collaborative Innovation Project of Shanghai Chest Hospital and the Science and Technology Development Project of Shanghai Municipality (No.19411963900 to FY). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The participants provided informed consent before taking part in the study. The study was approved by the Ethics Committee of Shanghai Chest Hospital (No. KS1972).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Doo KW, Yong HS, Kim HK, et al. Needlescopic resection of small and superficial pulmonary nodule after computed tomographic fluoroscopy-guided dual localization with radiotracer and hookwire. Ann Surg Oncol 2015;22:331-7. [Crossref] [PubMed]
- Suzuki K, Nagai K, Yoshida J, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest 1999;115:563-8. [Crossref] [PubMed]
- Wang YZ, Boudreaux JP, Dowling A, et al. Percutaneous localisation of pulmonary nodules prior to video-assisted thoracoscopic surgery using methylene blue and TC-99. Eur J Cardiothorac Surg 2010;37:237-8. [Crossref] [PubMed]
- Chen ZM, Xu JY, Cai WQ, et al. The 4-hook anchor coaxial needle with scaled suture is superior to the double spring coil for preoperative localization. J Thorac Dis 2021;13:4455-63. [Crossref] [PubMed]
- Finley RJ, Mayo JR, Grant K, et al. Preoperative computed tomography-guided microcoil localization of small peripheral pulmonary nodules: a prospective randomized controlled trial. J Thorac Cardiovasc Surg 2015;149:26-31. [Crossref] [PubMed]
- Fan W, Yang H, Ma J, et al. Indocyanine green fluorescence-navigated thoracoscopy versus traditional inflation-deflation approach in precise uniportal segmentectomy: a short-term outcome comparative study. J Thorac Dis 2022;14:741-8. [Crossref] [PubMed]
- Fumimoto S, Sato K, Koyama M, et al. Combined lipiodol marking and video-assisted thoracoscopic surgery in a hybrid operating room. J Thorac Dis 2018;10:2940-7. [Crossref] [PubMed]
- Mack MJ, Gordon MJ, Postma TW, et al. Percutaneous localization of pulmonary nodules for thoracoscopic lung resection. Ann Thorac Surg 1992;53:1123-4. [Crossref] [PubMed]
- Park CH, Han K, Hur J, et al. Comparative Effectiveness and Safety of Preoperative Lung Localization for Pulmonary Nodules: A Systematic Review and Meta-analysis. Chest 2017;151:316-28. [Crossref] [PubMed]
- Imperatori A, Nardecchia E, Cattoni M, et al. Perioperative identifications of non-palpable pulmonary nodules: a narrative review. J Thorac Dis 2021;13:2524-31. [Crossref] [PubMed]
- Kanazawa S, Ando A, Yasui K, et al. Localization of small pulmonary nodules for thoracoscopic resection: use of a newly developed hookwire system. Cardiovasc Intervent Radiol 1995;18:122-4. [Crossref] [PubMed]
- Iguchi T, Hiraki T, Gobara H, et al. CT fluoroscopy-guided preoperative short hook wire placement for small pulmonary lesions: evaluation of safety and identification of risk factors for pneumothorax. Eur Radiol 2016;26:114-21. [Crossref] [PubMed]
- Chen S, Zhou J, Zhang J, et al. Video-assisted thoracoscopic solitary pulmonary nodule resection after CT-guided hookwire localization: 43 cases report and literature review. Surg Endosc 2011;25:1723-9. [Crossref] [PubMed]
- Miyoshi K, Toyooka S, Gobara H, et al. Clinical outcomes of short hook wire and suture marking system in thoracoscopic resection for pulmonary nodules. Eur J Cardiothorac Surg 2009;36:378-82. [Crossref] [PubMed]
- Dendo S, Kanazawa S, Ando A, et al. Preoperative localization of small pulmonary lesions with a short hook wire and suture system: experience with 168 procedures. Radiology 2002;225:511-8. [Crossref] [PubMed]
- Ciriaco P, Negri G, Puglisi A, et al. Video-assisted thoracoscopic surgery for pulmonary nodules: rationale for preoperative computed tomography-guided hookwire localization. Eur J Cardiothorac Surg 2004;25:429-33. [Crossref] [PubMed]
- Seo JM, Lee HY, Kim HK, et al. Factors determining successful computed tomography-guided localization of lung nodules. J Thorac Cardiovasc Surg 2012;143:809-14. [Crossref] [PubMed]
- Ichinose J, Kohno T, Fujimori S, et al. Efficacy and complications of computed tomography-guided hook wire localization. Ann Thorac Surg 2013;96:1203-8. [Crossref] [PubMed]
- Fan L, Yang H, Yu L, et al. Multicenter, prospective, observational study of a novel technique for preoperative pulmonary nodule localization. J Thorac Cardiovasc Surg 2020;160:532-9.e2. [Crossref] [PubMed]
- Schulz KF, Altman DG, Moher D, et al. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [Crossref] [PubMed]
- Qi H, Wan C, Zhang L, et al. Early effective treatment of small pulmonary nodules with video-assisted thoracoscopic surgery combined with CT-guided dual-barbed hookwire localization. Oncotarget 2017;8:38793-801. [Crossref] [PubMed]
- Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011;63:S240-52. [Crossref] [PubMed]
- Iguchi T, Hiraki T, Matsui Y, et al. Short hookwire placement under imaging guidance before thoracic surgery: A review. Diagn Interv Imaging 2018;99:591-7. [Crossref] [PubMed]
- Wicky S, Dusmet M, Doenz F, et al. Computed tomography-guided localization of small lung nodules before video-assisted resection: experience with an efficient hook-wire system. J Thorac Cardiovasc Surg 2002;124:401-3. [Crossref] [PubMed]
- Cantey EP, Walter JM, Corbridge T, et al. Complications of thoracentesis: incidence, risk factors, and strategies for prevention. Curr Opin Pulm Med 2016;22:378-85. [Crossref] [PubMed]
- Iguchi T, Hiraki T, Gobara H, et al. Retained Short Hook Wires Used for Preoperative Localization of Small Pulmonary Lesions During Video-Assisted Thoracoscopic Surgery: A Report of 2 Cases. Cardiovasc Intervent Radiol 2015;38:1376-9. [Crossref] [PubMed]
- Yi JH, Choi PJ, Bang JH, et al. Systemic air embolism after computed tomography-guided hook wire localization: two case reports and literature review. J Thorac Dis 2018;10:E59-64. [Crossref] [PubMed]


