Is surgery still the optimal treatment for stage I non-small cell lung cancer?
We find ourselves at a time in history when we can no longer state with certainty that surgery is the optimal treatment for patients with operable stage I non-small cell lung cancer (NSCLC) (1). Although published guidelines continue to assert that surgery is still the “standard of care” (2,3), mounting evidence now suggests that stereotactic ablative radiotherapy (SABR), also known as stereotactic body radiotherapy (SBRT), might actually be an equivalent or, on occasion, even a preferred option as demonstrated by recent published randomized study (STARS and ROSEL) (4).
For now, there is no enough evidence that can support the belief that SBRT is uniformly as effective as surgery, let alone better. However, promising results published in recent decades have already begun to change practice. With reports of treatment-related mortality rates as low as 0% with SBRT in the frail and elderly (5), patients and referring physicians are increasingly refusing surgical resection. The largest cohort of operable patients treated with SBRT now exceeds 660 with a reported 3-year overall survival (OS) of 77–80% (6). Next, there is prospective phase II clinical trial evidence that demonstrates the 5-year local control rate is as high as 93% (7). While these results, in general, compare favorably with surgical series, and are furthermore corroborated by matched-pair analyses that suggests equivalent survival with either treatment (8), they are not yet convincing enough to compel a change in evidence-based recommendations that maintain surgery is always the preferred option (2,3). Numerous editorials have shed light on the biases of retrospective comparisons and recently highlighted the limitations of a widely discussed pooled analysis of two prematurely terminated phase III randomized trials that reported a statistically significant OS benefit at 3-year with SBRT when compared to patients randomized to lobectomy (9-12).
If SBRT is potentially as effective as, or even better than, surgery, then why haven’t expert panels yet acknowledged that it is an acceptable alternative standard of care? To better understand the predicament, an examination of the history of lung cancer surgery more than half a century ago is instructive. It suggests the dominance of surgery emerged through the happenstance of history, never to be successfully challenged by any promising alternative strategies.
Lung cancer surgery emerged as the only hope for cure in the 1930’s during the height of enthusiasm for radical surgery. Following the turn of the 20th century, Halsted’s radical mastectomy inspired Crile’s radical neck dissection (13) and Brunschwig’s complete pelvic exenteration [1948] (14). Brilliant surgeons of that time, often devoted to Halsted’s theory of centrifugal tumor spread (15), focused their strategies toward achieving wider and wider margins. The consequence of this paradigm culminated with Starzl’s introduction of the abdominal organ cluster transplantation for gastrointestinal tumors involving multiple organs [1989], capturing one of the most extreme developments of radical surgery aside from hemicorporectomy (16). Its development was particularly intriguing given Bernard Fisher’s NSABP B-04 study was published more than a decade earlier [1977], disproving the century old belief that tumors spread primarily to distant sites only through direct invasion of adjacent tissue and lymphatic channels (17), which included similar beliefs regarding the mechanism of metastases for lung cancer (18).
The initial reports of surgery for lung cancer date back to 1913 (19). Its value was initially in doubt, since no survivors beyond 1 year were reported in the literature (20). This would eventually change several decades later following advances in anesthesia, blood transfusions, and nutritional support that helped Evarts Graham pioneer the pneumonectomy at Washington University in St. Louis [1933] (20). The development of this procedure helped immortalize Dr. Graham among the ranks of other prominent surgeons of that era (19). The patient in that report survived almost 30 years and served as a living symbol of the courage and fortitude of thoracic surgeons who were the first physicians in history to provide a curative treatment for patients with lung cancer (19). Such an extensive resection for a tumor that measured only 1 cm in diameter had been deemed necessary, but not only because it was located near the bifurcation of the left proximal bronchial tree. As Graham and Singer explained in their initial report, the procedure was performed during a time in history when it was widely accepted that there were no other options that held promise. As they wrote, there was “no record in the literature of the successful treatment by radiotherapy of a single case in which pathological evidence has been incontrovertible and which a five year interval without recurrence has elapsed between the treatment and the time of reporting the case, despite the fact that many cases have been treated according to the most modern methods of using both X-ray and radium” (20).
Soon thereafter, and without randomized trials, surgery was inaugurated as the ideal treatment for lung cancer that should be considered for any patient potentially fit for surgery. By the following decade, reports declared that the technical obstacles of lung cancer surgery had been surmounted to overcome the operative mortality rates that at first appeared formidable (21). This was despite disappointing survival rates of only 21–32% (22). In a landmark essay published in 1946, Edward Churchill, who was then the Chief of General Surgical Services at Massachusetts General Hospital, forecast a promising outlook for lung cancer treatment that focused on advances in surgery, while referencing radiotherapy as a futile option with little contribution to survival or relief of those who were suffering (21). It was widely believed that radiotherapy should be reserved for surgical rejects (23), and comments that it was “worse than useless” are found in the literature (24). There was some truth to this, as the decades between 1920–1940 have since been considered a forgotten period during which radiotherapists were at times distracted with a concern for fatal electrocution by their poorly insulated X-ray systems (25). After all, this was an era that predated Hoff’s development of the microprocessor in 1971, and Hounsfield’s invention of the CT scanner in 1977, each an innovation that would revolutionize the field of radiation oncology (26). Despite these challenges, studies in the 1950’s had already demonstrated that radiotherapy could achieve long-term tumor eradication (27). It was not be long before authors suggested that survival rates after radiotherapy might actually be similar to surgical series (22). It’s notable that this became apparent even in an era during which radiotherapy techniques were antiquated and the general health of patients referred for radiotherapy was often poor (28,29).
By the 1960’s, a randomized trial was performed to prospectively compare surgery to radiotherapy (30). The study included patients with grossly enlarged mediastinal lymph nodes visible on chest X-ray. Radiotherapy utilized supervoltage photons to deliver 4,500 rad units over 4 weeks of daily treatment (a dose that is now established as suboptimal, delivered with an antiquated technique that predated the modern linear accelerator). Fifty-eight patients were randomized, a sample size similar to the recently published pooled analysis of the STARS and ROSEL trials. Although survival was estimated to be only 7–23% at 4 years with surgery, this outcome was superior to the radiotherapy group with borderline statistical significance. The results of this prospective comparison were widely influential at the time and firmly established surgery as the standard of care for the foreseeable future.
As a consequence, best practices in primary care recommended an expeditious referral for thoracic surgery consultation whenever a patient was suspected of harboring lung cancer confined to the chest. This paradigm ensured surgeons had the first right of refusal to offer a resection, and fostered an era of gatekeeping that may have impeded the recruitment of lung cancer patients onto randomized clinical trials in subsequent decades (23). It helped amass an impressive body of literature that eventually demonstrated surgeons could carefully select ideal patients who could tolerate surgery such that 19 out of 20 patients could survive a resection beyond 90 days (31). Long-term outcomes gradually improved and 5-year survival rates approached 80% in highly selected patients (32). However, such outcomes were not often reproduced as most series instead reported 5-year survival rates between 58–77% (33-35). By the 1990’s, referring physicians questioned whether the long-held view that surgery prolongs the life of lung cancer patients may have merely been an artifact of selection bias; they offered an alternative hypothesis that many of these patients would have lived just as long with observation (36). Eventually, the publication of the National Lung Screening Trial in 2011 provided convincing data that surgery improves survival, as 92.5% of stage I patients in that study underwent surgery (37). These data had demonstrated that the resection of lung cancers that were detected earlier with annual chest CTs, as compared to annual chest X-ray, reduced lung cancer mortality by 20%. A renewed belief that surgery prolongs survival was an instrumental aspect of the US Preventive Taskforce recommendations to endorse chest CT screening in high risk patients (38).
Today, the field of radiation oncology has emerged out of the black and white era of technology following milestones in medical physics, computer science, and engineering (39,40). Important developments in imaging and tumor targeting have vastly improved the accuracy of radiotherapy, allowing escalation of daily doses to levels not previously considered practicable or safe (Figure 1). These advancements laid the foundation for the initial National Cancer Institute funded dose-escalation trial led by Timmerman et al. that opened in 2000 and enrolled patients at the University of Indiana and the Richard A. Roudebush Veterans Affairs Medical Center in Indianapolis (26). The observation of tumor control rates exceeding 90% was serendipitous and simply unprecedented at the time. As these results were readily reproducible around the world using a variety of different radiation therapy treatment systems (41), referring physicians increasingly recommended SBRT for operable patients and the survival outcomes that emerged soon paralleled that of surgical series (Table 1). It is perhaps this body of literature, more than others, that now squarely challenges the belief that surgery is still the optimal treatment for stage I NSCLC.

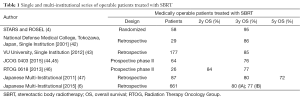
Full table
Yet, as promising as SBRT may appear, the data available today remain premature to exclude the possibility that surgery is still the optimal treatment option for many patients. It may be tempting, and even seem more ethical at times, to counsel a patient towards selecting SBRT to avoid the risks of an operation and need for hospitalization. However, without high level evidence directly comparing the long-term outcomes of these disparate treatments, the only scientifically accurate conclusion one can make at present about this subject is that “we no longer know which treatment is better”. The reader, who may have a preference to rely on guideline recommendations, and be accustomed to deferring critical thought to expert opinions, may find this statement unsettling. However, those who suggest surgery is the only standard of care are increasingly considered to be potentially misleading (1). This dilemma is real, and has brought referring physicians to a crossroads. Primary care physicians, pulmonologists, and patient advocates are increasingly finding it difficult to omit discussions about SBRT as an alternative to surgery. Patients are also increasingly perplexed, particularly for those who have learned through the media that there is a promising non-surgical option to “zap” lung tumors with SBRT instead (48,49). Many are increasingly learning that both preclinical and clinical data now suggest that SBRT, not surgery, activates cancer specific immune responses by releasing tumor associated antigens from killed cancer cells that could function as an effective in situ cancer vaccine (50,51). It is therefore clear that this clinical question warrants the additional resources needed to eventually complete a prospective randomized trial, despite three prior unsuccessful attempts [ROSEL, STARS, ACOSOG-4099/Radiation Therapy Oncology Group (RTOG)-1021] (52).
In good news, while the first set of phase III trials that aimed to randomize patients between surgery and SBRT closed due to poor accrual in 2013, a new set of prospective studies are now funded to try once again (Table 2). The commitment of each study’s sponsor is a testament to the significance that many physicians, patient, and advocacy groups have placed on discovering the optimal management strategy for stage I NSCLC. The potential clearly exists that these studies will find certain pre-treatment characteristics that can better predict which patients are better served with surgery, SBRT, or either. However, until we have balanced cohorts of patients randomized between these two treatments, patients and physicians will only be able to hypothesize when surgery is the optimal treatment, or not.
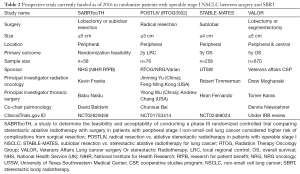
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Treasure T, Rintoul RC, Macbeth F. SABR in early operable lung cancer: time for evidence. Lancet Oncol 2015;16:597-8. [Crossref] [PubMed]
- Ettinger DS, Wood DE, Akerley W, et al. Non-small cell lung cancer, version 1.2015. J Natl Compr Canc Netw 2014;12:1738-61. [PubMed]
- Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e211S-50S.
- Chang JY, Senan S, Paul MA, et al. Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Oncol 2015;16:630-7. [Crossref] [PubMed]
- Palma D, Lagerwaard F, Rodrigues G, et al. Curative treatment of Stage I non-small-cell lung cancer in patients with severe COPD: stereotactic radiotherapy outcomes and systematic review. Int J Radiat Oncol Biol Phys 2012;82:1149-56. [Crossref] [PubMed]
- Komiyama T, Onishi H, Shioyama Y, et al. Japanese Multicenter Study of Stereotactic Body Radiotherapy for 661 Medically Operable Patients with Stage I Non-Small Cell Lung Cancer. J Thorac Oncol 2015;10:ORAL19.05. Available online: file:///C:/Users/Administrator/Desktop/ETOP%20WCLC%202015_collated_Final.pdf
- Timmerman RD, Hu C, Michalski J, et al. Long-term Results of RTOG 0236: A Phase II Trial of Stereotactic Body Radiation Therapy (SBRT) in the Treatment of Patients with Medically Inoperable Stage I Non-Small Cell Lung Cancer. International Journal of Radiation Oncology • Biology • Physics 2014;90:S30.
- Shirvani SM, Jiang J, Chang JY, et al. Lobectomy, sublobar resection, and stereotactic ablative radiotherapy for early-stage non-small cell lung cancers in the elderly. JAMA Surg 2014;149:1244-53. [Crossref] [PubMed]
- Cao C, D'Amico T, Demmy T, et al. Surgery versus SABR for resectable non-small-cell lung cancer. Lancet Oncol 2015;16:e370-1. [Crossref] [PubMed]
- Hamaji M, Groth SS, Sugarbaker DJ, et al. Surgery versus SABR for resectable non-small-cell lung cancer. Lancet Oncol 2015;16:e372. [Crossref] [PubMed]
- Meyers BF, Puri V, Broderick SR, et al. Lobectomy versus stereotactic body radiotherapy for stage I non-small cell lung cancer: Post hoc analysis dressed up as level-1 evidence? J Thorac Cardiovasc Surg 2015;150:468-71. [Crossref] [PubMed]
- Jones DR. Do we know bad science when we see it? J Thorac Cardiovasc Surg 2015;150:472-3. [Crossref] [PubMed]
- Silver CE, Rinaldo A, Ferlito A. Crile's neck dissection. Laryngoscope 2007;117:1974-7. [Crossref] [PubMed]
- Brunschwig A. Complete excision of pelvic viscera for advanced carcinoma; a one-stage abdominoperineal operation with end colostomy and bilateral ureteral implantation into the colon above the colostomy. Cancer 1948;1:177-83. [Crossref] [PubMed]
- Halsted WS. I. The Results of Radical Operations for the Cure of Carcinoma of the Breast. Ann Surg 1907;46:1-19. [Crossref] [PubMed]
- Starzl TE, Todo S, Tzakis A, et al. Abdominal organ cluster transplantation for the treatment of upper abdominal malignancies. Ann Surg 1989;210:374-85; discussion 385-6. [Crossref] [PubMed]
- Fisher B, Montague E, Redmond C, et al. Comparison of radical mastectomy with alternative treatments for primary breast cancer. A first report of results from a prospective randomized clinical trial. Cancer 1977;39:2827-39. [Crossref] [PubMed]
- Onuigbo WI. Centrifugal metastasis in lung cancer. Br J Dis Chest 1961;55:86-90. [Crossref] [PubMed]
- Horn L, Johnson DH, Evarts A. Graham and the first pneumonectomy for lung cancer. J Clin Oncol 2008;26:3268-75. [Crossref] [PubMed]
- Graham EA, Singer JJ. Successful removal of an entire lung for carcinoma of the bronchus. JAMA 1933;101:1371-4. [Crossref] [PubMed]
- Churchill ED. Primary carcinoma of the lung. J Am Med Assoc 1948;137:455-61. [Crossref] [PubMed]
- Smart J, Hilton G. Radiotherapy of cancer of the lung; results in a selected group of cases. Lancet 1956;270:880-1. [Crossref] [PubMed]
- Timmermann C. As depressing as it was predictable? Lung cancer, clinical trials, and the Medical Research Council in postwar Britain. Bull Hist Med 2007;81:312-34. [Crossref] [PubMed]
- SHORVON LM. Carcinoma of the bronchus with especial reference to its treatment by radiotherapy. Br J Radiol 1947;20:443-9. [Crossref] [PubMed]
- Kemerink GJ, Kütterer G, Wright A, et al. Forgotten electrical accidents and the birth of shockproof X-ray systems. Insights Imaging 2013;4:513-23. [Crossref] [PubMed]
- Timmerman R, Papiez L, McGarry R, et al. Extracranial stereotactic radioablation: results of a phase I study in medically inoperable stage I non-small cell lung cancer. Chest 2003;124:1946-55. [Crossref] [PubMed]
- Burnett HW Jr, Steinberg I, Dotter CT. Seven-year survival after radiation therapy in a patient with inoperable cancer of the lung. N Engl J Med 1952;247:850-1. [Crossref] [PubMed]
- Leddy ET. Roentgen therapy of bronchiogenic carcinoma. Minn Med 1947;30:975-7. [PubMed]
- Jacobsen VC. Complications of deep X-ray therapy of carcinoma of the lung. Am J Med 1948;5:148-56. [Crossref] [PubMed]
- Morrison R, Deeley TJ, Cleland WP. The Treatment of Carcinoma of the Bronchu: A Clinical Trial to Cmopare Surgery and Supervoltage Radiotherapy. Lancet 1963;281:683-4. [Crossref]
- Senthi S, Senan S. Surgery for early-stage lung cancer: post-operative 30-day versus 90-day mortality and patient-centred care. Eur J Cancer 2014;50:675-7. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS. Survival of patients with true pathologic stage I non-small cell lung cancer. Ann Thorac Surg 2009;88:917-22; discussion 922-3. [Crossref] [PubMed]
- Zheng X, Schipper M, Kidwell K, et al. Survival outcome after stereotactic body radiation therapy and surgery for stage I non-small cell lung cancer: a meta-analysis. Int J Radiat Oncol Biol Phys 2014;90:603-11. [Crossref] [PubMed]
- Rami-Porta R, Crowley JJ, Goldstraw P. The revised TNM staging system for lung cancer. Ann Thorac Cardiovasc Surg 2009;15:4-9. [PubMed]
- Chang MY, Mentzer SJ, Colson YL, et al. Factors predicting poor survival after resection of stage IA non-small cell lung cancer. J Thorac Cardiovasc Surg 2007;134:850-6. [Crossref] [PubMed]
- Lederle FA, Niewoehner DE. Lung cancer surgery. A critical review of the evidence. Arch Intern Med 1994;154:2397-400. [Crossref] [PubMed]
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Moyer VA; U.S. Preventive Services Task Force. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2014;160:330-8. [PubMed]
- Timmerman RD, Herman J, Cho LC. Emergence of stereotactic body radiation therapy and its impact on current and future clinical practice. J Clin Oncol 2014;32:2847-54. [Crossref] [PubMed]
- Timmerman R, Papiez L, Suntharalingam M. Extracranial stereotactic radiation delivery: expansion of technology beyond the brain. Technol Cancer Res Treat 2003;2:153-60. [PubMed]
- Guckenberger M. Stereotactic body radiotherapy for stage I NSCLC: the challenge of evidence-based medicine. J Thorac Oncol 2014;9:e17-8. [Crossref] [PubMed]
- Uematsu M, Shioda A, Suda A, et al. Computed tomography-guided frameless stereotactic radiotherapy for stage I non-small cell lung cancer: a 5-year experience. Int J Radiat Oncol Biol Phys 2001;51:666-70. [Crossref] [PubMed]
- Lagerwaard FJ, Verstegen NE, Haasbeek CJ, et al. Outcomes of stereotactic ablative radiotherapy in patients with potentially operable stage I non-small cell lung cancer. Int J Radiat Oncol Biol Phys 2012;83:348-53. [Crossref] [PubMed]
- Nagata Y, Hiraoka M, Shibata T, et al. A phase II trial of stereotactic body radiation therapy for operable T1N0M0 non-small cell lung cancer: Japan Clinical Oncology Group (JCOG0403). Int J Radiat Oncol Biol Phys 2010;78:S27-8. [Crossref]
- Nagata Y, Hiraoka M, Shibata T, et al. Prospective Trial of Stereotactic Body Radiation Therapy for Both Operable and Inoperable T1N0M0 Non-Small Cell Lung Cancer: Japan Clinical Oncology Group Study JCOG0403. Int J Radiat Oncol Biol Phys 2015;93:989-96. [Crossref] [PubMed]
- Timmerman RD, Paulus R, Pass HI, et al. RTOG 0618: Stereotactic body radiation therapy (SBRT) to treat operable early stage lung cancer patients. J Clin Oncol 2013;31:abstr 7523.
- Onishi H, Shirato H, Nagata Y, et al. Stereotactic body radiotherapy (SBRT) for operable stage I non-small-cell lung cancer: can SBRT be comparable to surgery? Int J Radiat Oncol Biol Phys 2011;81:1352-8. [Crossref] [PubMed]
- Gupta S. Zapping Tumor Effective for Stage I Non-Small Cell Lung Cancer. Available online: , 2015.http://www.medpagetoday.com/HematologyOncology/LungCancer/51630
- Rice D, Sepesi B, Heymach J, et al. SABR vs surgery for NSCLC in the media. Lancet Oncol 2015;16:e422. [Crossref] [PubMed]
- Aerts JG, De Goeje P, Schram M, et al. MINI18.03—immune activation in early stage non-small cell lung cancer (NSCLC) following stereotactic ablative radiotherapy (SABR) and surgery (ID 2123). 16th World Conference on Lung Cancer; Denver, CO, USA; Sept 6–9, 2015.
- Bernstein MB, Krishnan S, Hodge JW, et al. Immunotherapy and stereotactic ablative radiotherapy (ISABR): a curative approach? Nat Rev Clin Oncol 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Moghanaki D, Karas T. Surgery versus SABR for NSCLC. Lancet Oncol 2013;14:e490-1. [Crossref] [PubMed]


