
Patterns and outcome of unplanned care in lung cancer patients: an observational study in a medical oncology department
Highlight box
Key findings
• In our lung cancer cohort the 1-year cumulative incidence for emergency consultation and for un-planned hospital admission was 71.3% and 56.7%, respectively. Eighty percent of unplanned care were related to cancer or its treatment.
What is known and what is new?
• Current evidence is heterogeneous, describing a wide range for burden and risk of acute care needs.
• We assessed the need for unplanned care of lung cancer patients, establishing outcome and quality measures to benchmarking improvement interventions. The factors associated with the theoretically unpredictable demand for care were described.
What is the implication, and what should change now?
• Unplanned care for lung cancer patients must be considered in the management of oncology services; our study shows that it is measurable and evaluable. It is necessary to implementing technologies for a more in-depth analysis of medical records to develop a continuous learning process based on daily care.
Introduction
Lung cancer is the second most common neoplasm and the leading cause of mortality worldwide, with 2.2 million new diagnoses and 1.8 million deaths per year (1). These data define the magnitude of the health problem, although they are insufficient to illustrate its impact on morbidity and health resource consumption. There is increasing interest in unplanned hospital care utilization among lung cancer patients to understand disease morbidity and identify continuity of care gaps (2,3).
Consultation in the emergency department (ED) and unplanned hospitalization admission are disruptive events in the patient’s disease, often caused by symptoms or complications associated with the cancer itself or toxicity of treatments (4). In some cases, given that more than 44% of lung cancer patients are diagnosed with metastatic disease (5), the ED is the entry door to the final diagnosis (6). Small cell lung cancer is especially prone to this situation (7). The ED is the origin of the majority of hospital admissions for cancer patients (8), with admission rates higher than noncancer emergencies, ranging between 28.8% and 90% (9-11), being one of the most important sources of expenditure and variability of expenditure for health systems (12), with a significant consumption of resources due to hospitalization. A study of economic burden of cancer across the European Union attribute 56% of all estimated costs associated with cancer treatment to ED attendance and subsequent hospitalization (13).
Reduction of unplanned acute care is a major priority for clinical transformation in oncology (14), and its evaluation and definition allow the identification and characterization of areas for quality improvement. Despite being measurable (15), the available studies are limited and heterogeneous, describing a wide range of ED consultations, 6–83% (16), and hospitalization admissions, 16–71%, with differences depending on the tumor, stage, population subgroup, and period studied (8,17-19). Clinical trials are not the best source to evaluate unplanned care, observing a consistently lower hospitalization rate than in real-world cohort studies (16,17). In this scenario, real-world data may be of special interest to address relevant clinical and policy questions that cannot be answered using clinical trial data (20), such as acute care performance and access for lung cancer patients.
We aim to describe the risk and burden of unplanned care, ED visits and unplanned hospital admissions during the lung cancer care process in a medical oncology department of a tertiary hospital, as well as the modifying factors that determine acute care. We integrated activity and administrative data extracted from the Electronic Medical Record (1.2 million records) together with clinical data from a lung cancer registry that was curated into a new structured database, to identify and measure the acute care needs of patients. We present this article in accordance with the STROBE reporting checklist (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-23-48/rc).
Methods
Study design and population
This was an observational retrospective cohort study that included all lung cancer patients, all stages and histologies, treated by the Medical Oncology Department at Puerta de Hierro-Majadahonda University Hospital (PHUH), a public teaching hospital reference for a population of 500,000 inhabitants, between January 1st 2016 and December 31st 2020 (5 consecutive years). Patients diagnosed with lung cancer referred directly to a palliative care unit after diagnosis without being assessed by the Medical Oncology Department were excluded. Follow-up data cut off was settled on June 30th 2021. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the institutional ethics board of Puerta de Hierro-Majadahonda University Hospital, Madrid (No. PI_175_20). Because of the retrospective design of the study and deidentified data, informed consent from all participants was waived.
Data sources
Patients were identified from the PHUH tumor registry, which includes the following variables: cancer diagnosis, sex, birth date, diagnosis date, cancer site, and stage. Data was expanded by reviewing individual patient records, adding clinical and pathological variables: history of personal and family cancer, history of smoking, CHARLSON comorbidity score, Eastern Cooperative Oncology Group performance status (ECOG PS), drugs used and symptoms at first consultation, histology and molecular studies carried out, follow-up status and date of relapse and death.
The information on care throughout the oncological process was obtained from administrative data: extracted from the data warehouse system of the Electronic Medical Record, between January 1st, 2016 and June 30th, 2021, we identified 121,878 medical oncology appointments, 881,738 emergency service attendance, 140,432 hospital admissions, and 62,277 records for systemic treatments administered. Data obtained was cross-referenced using the hospital identification number with the study cohort previously selected from the tumor registry, obtaining the variables: date of first medical oncology visit, date and time of ED visits and hospital admissions; reason and origin of ED consultation (referring physician); ED time of attendance (times among hospital arrival, triage, medical attention, and resolution); triage classification according to the Manchester Triage System (MTS) (21), and hospital admissions diagnoses coded by the International Classification of Diseases (ICD-10).
Healthcare activity data were obtained through Oracle Business Intelligence Discoverer 10 g Version 2 (10.1.2.1). For data preparation, crossing and depuration Stata v.16 was used.
Outcomes
The main objective of the study was to assess the incidence of unplanned care, ED visits and unplanned hospital admissions, from the first visit to the medical oncology service and its potential conditioning variables. Admissions for planned chemotherapy, radiotherapy or surgery were excluded.
As secondary objectives, a description and a quality of unplanned care evaluation was carried out. Measures and indicators used for ED visits were: reason and origin of ED consultation (referring physician), day and hour of care, time from hospital arrival to classification, time from classification to medical evaluation according to the MTS recommended times (21), admission rate and total time from hospital arrival to resolution (discharge or admission). For unplanned admissions: admission to the Oncology Hospitalization Unit, length of stay, mortality during admission, readmission rate at 30 days, reasons for admission and total cost of hospitalization for the entire cohort of lung cancer patients using the values specified by the Spanish National Health System for each diagnosis related group.
Statistical analysis
The categorical variables are described by absolute and relative frequencies, and for quantitative variables, we used the mean (standard deviation) or median (percentiles 25 and 75). Comparisons of numerical variables were performed using Student’s t test, while categorical variables were compared by performing the chi-squared test. A P value <0.05 was considered significant. An analysis of time from the first consultation in Medical Oncology to the first consultation in the ED and until the first unplanned admission was carried out by means of survival analysis techniques. Time to event was analyzed considering patient death as a competitive event in the observation of both outcomes; therefore, the cumulative incidence function (CIF) is shown instead of Kaplan-Meier estimates. Fine & Gray competing risk regression was performed to establish the association of variables with time to event (22). The subhazard ratio (SHR) with its corresponding 95% confidence intervals (95% CI) are shown as effect sizes. We assume that missing data are missing completely at random, so we performed a complete case analysis. Statistical analysis was performed using Stata v.16.
Results
Between January 1st, 2016, and December 31st, 2020, 933 lung cancer patients were identified in the PHUH tumor registry, 112 patients were excluded as described in the flow diagram (Figure 1), and 821 consecutive patients with lung cancer, comprising all histologies and stages, were evaluated in the Medical Oncology Department and therefore included. At the data cut-off, the median follow-up was 32.8 months (95% CI: 30.5–36.7). A total of 681 patients required consultation in the ED (82.9%; 95% CI: 80.2–85.4%), and 558 required an unplanned hospitalization admission (68%; 95% CI: 64.6–71.1%). Patient characteristics, rates of ED consultation and unplanned admissions are described in Table 1.

Table 1
| Characteristics | Total | Emergency visits, n (%) | Unplanned hospital admissions, n (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Emergency consultation | No emergency visit | P | Unplanned admissions | No admissions | P | ||||
| All population | 821 | 681 (82.9) | 140 (17.1) | 558 (68.0) | 263 (32.0) | ||||
| Sex | 0.593 | 0.036 | |||||||
| Male | 553 | 456 (82.5) | 97 (17.5) | 389 (70.3) | 164 (29.7) | ||||
| Female | 268 | 225 (84.0) | 43 (16.0) | 169 (3.1) | 99 (36.9) | ||||
| Age | 0.671 | 0.903 | |||||||
| <50 years | 41 | 32 (78.0) | 9 (22.0) | 26 (63.4) | 15 (36.6) | ||||
| 50–64 years | 297 | 249 (83.8) | 48 (16.2) | 201 (67.7) | 96 (32.3) | ||||
| 65–74 years | 310 | 260 (83.9) | 50 (16.1) | 214 (69.0) | 96 (31.0) | ||||
| >74 years | 173 | 140 (80.9) | 33 (19.1) | 117 (67.6) | 56 (32.4) | ||||
| Tobacco use | 0.515 | 0.031 | |||||||
| Never smoker | 70 | 56 (80.0) | 14 (20.0) | 38 (54.3) | 32 (45.7) | ||||
| Former smoker | 380 | 313 (82.4) | 67 (17.6) | 260 (68.4) | 120 (31.6) | ||||
| Active smoker | 367 | 311 (84.7) | 56 (15.3) | 258 (70.3) | 109 (29.7) | ||||
| Charlson Comorbidity Index | 0.027 | <0.001 | |||||||
| ≤6 | 251 | 197 (78.5) | 54 (21.5) | 140 (55.8) | 111 (44.2) | ||||
| ≥7 | 566 | 480 (84.8) | 86 (15.2) | 415 (73.3) | 151 (26.7) | ||||
| ECOG PS scale score | <0.001 | <0.001 | |||||||
| 0 | 170 | 134 (78.8) | 36 (21.2) | 92 (54.1) | 78 (45.9) | ||||
| 1 | 380 | 322 (84.7) | 58 (15.3) | 248 (65.3) | 132 (34.7) | ||||
| 2 | 157 | 144 (91.7) | 13 (8.3) | 136 (86.6) | 21 (13.4) | ||||
| 3–4 | 108 | 77 (71.3) | 31 (28.7) | 78 (72.2) | 30 (27.8) | ||||
| Histology | 0.011 | 0.030 | |||||||
| NSCLC | 650 | 528 (81.2) | 122 (18.8) | 430 (66.2) | 220 (33.8) | ||||
| SCLC | 171 | 153 (89.5) | 18 (10.5) | 128 (74.9) | 43 (25.1) | ||||
| NSCLC subtype | 0.949 | 0.627 | |||||||
| Adenocarcinoma | 397 | 324 (81.6) | 73 (18.4) | 257 (64.7) | 140 (35.3) | ||||
| Squamous cell | 182 | 147 (80.8) | 35 (19.2) | 124 (68.1) | 58 (31.9) | ||||
| NOS/other | 71 | 57 (80.3) | 14 (19.7) | 49 (69.0) | 22 (31.0) | ||||
| Stage at diagnosis | <0.001 | <0.001 | |||||||
| IA–IIB | 97 | 65 (67.0) | 32 (33.0) | 39 (40.2) | 58 (59.8) | ||||
| IIIA–IIIB | 201 | 169 (84.1) | 32 (15.9) | 128 (63.7) | 73 (36.3) | ||||
| IVA–IVB | 523 | 447 (85.5) | 76 (14.5) | 391 (74.8) | 132 (25.2) | ||||
| NSCLC IV | 0.598 | 0.001 | |||||||
| Driver mutation | 64 | 53 (82.8) | 11 (17.2) | 36 (56.2) | 28 (43.8) | ||||
| Not driver mutation | 342 | 292 (85.4) | 50 (14.6) | 260 (76.0) | 82 (24.0) | ||||
| Symptoms at diagnosis | P value for symptom present/symptom absent comparison | ||||||||
| Cough | 372 | 309 (83.1) | 63 (16.9) | 0.987 | 255 (68.6) | 117 (31.4) | 0.765 | ||
| Dyspnoea | 310 | 260 (83.9) | 50 (16.1) | 0.641 | 228 (73.6) | 82 (26.4) | 0.008 | ||
| Pain | 319 | 285 (89.3) | 34 (10.7) | <0.001 | 247 (77.4) | 72 (22.6) | <0.001 | ||
| Weight loss | 261 | 223 (85.4) | 38 (14.6) | 0.219 | 194 (74.3) | 67 (25.7) | 0.008 | ||
| Drugs at diagnosis | P value for drug use/not use comparison | ||||||||
| Opioids | 183 | 160 (87.4) | 23 (12.6) | 0.070 | 146 (79.8) | 37 (20.2) | <0.001 | ||
| Steroids | 202 | 172 (85.2) | 30 (14.8) | 0.350 | 160 (79.2) | 42 (20.8) | <0.001 | ||
| Metastasis location | P value for metastatic location affected/not affected comparison | ||||||||
| Liver | 128 | 108 (84.4) | 20 (15.6) | 0.631 | 107 (83.6) | 21 (16.4) | <0.001 | ||
| Bone | 226 | 193 (85.4) | 33 (14.6) | 0.246 | 171 (75.7) | 55 (24.3) | 0.004 | ||
| Pleural | 163 | 138 (84.7) | 25 (15.3) | 0.511 | 130 (79.7) | 33 (20.3) | <0.001 | ||
| CNS | 124 | 107 (86.3) | 17 (13.7) | 0.272 | 94 (75.8) | 30 (24.2) | 0.044 | ||
ECOG PS, Eastern Cooperative Oncology Group Performance Status; NSCLC, non-small cell lung cancer; SCLC, small cell lung cancer; NOS, not otherwise specified; CNS, central nervous system.
Emergency visits
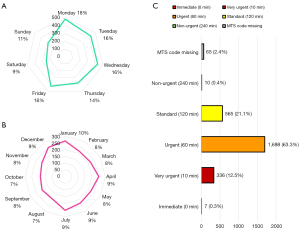
For the total population, 2,681 emergency visits were identified. In 14.6% of the consultations, the patients were referred to ED by their oncologist, 4.2% were referred by their primary care physician, 74.7% visit ED on their own needs, while 6.5% were transferred after evaluation by emergency services at the patient’s home. Fifty-eight percent of the ED visits were from 8:00 a.m. to 3:00 p.m., 31% from 3:00 p.m. to 10:00 p.m. and 11% on the night shift, from 10:00 p.m. to 8:00 a.m. The highest proportion of visits were on working days, and the days with the highest and lowest care burden were Monday with 18% of the ED visits and Saturday with 9% (Figure 2A). The distribution of ED consultations was similar among different months of the year (Figure 2B). The median time and interquartile range (IQR) from hospital arrival to emergency triage was 7 min (IQR, 4–12 min). In the triage, the reason for consultation was considered to be related to cancer or treatment-related complications in 86% of ED visits. The symptoms most frequently referred to as the reason for consultation on arrival at the ED were dyspnea, 20.4%, and pain, 15.2%. The classification of the need for attention according to the MTS was as follows: 0.3% immediate, 12.5% very urgent, 63.3% urgent, 21.1% standard, 0.4% nonurgent, and 2.4% of ED visits had their MTS code missing (Figure 2C). The quality indicators: attention time and resolution time according to the level of MTS, as well as the admission rate are described in Figure 3.

Unplanned hospital admission
A total of 1,186 unplanned admissions were identified, 6.2%, 26.1% and 67.7% corresponding to patients with stages I–IIB, IIIA–IIIC and IVA–IVB, respectively. A total of 97.7% were admitted from the ED, and 85.2% of the admissions were at the Oncology Hospitalization Unit. The median length of stay was 6 days (IQR, 3–10 days), mortality 17.3% (88.6% related to disease progression; 1.5% attributed to treatment side-effects), and 30-day readmission rate 23.3%. Quality indicators by stage are shown in Table 2. When evaluating the diagnoses coded for each admission record, the neoplasia is considered related to the admission in 80.9% of the unplanned admissions. An infection was diagnosed in 33.4% of the hospitalizations, respiratory failure in 19.3%, a metabolic disorder in 14.5%, pleural effusion in 10.2%, a neurological event in 9.6% and pain control need in 7.6%. We also observed a diagnosis coded as treatment-related toxicity in 29.8% of admissions. The direct cost attributed to unplanned admissions in the study period for the entire cohort, based on the reference prices for the diagnosis related group that codes each admission, amounted to 6,280,006 €.
Table 2
| Tumor stage | Unplanned hospital admissions, n (%) | % of admissions in Oncology Unit | Median days of length of stay [IQR] | Mortality, % | 30-days readmissions rate, % |
|---|---|---|---|---|---|
| Stage IA–IIB | 74 (6.2) | 50 | 6 [3–13] | 7.5* | 10.7 |
| Stage IIIA–IIIC | 309 (26.1) | 80.3 | 6 [3–10] | 12.7* | 21.7 |
| Stage IVA–IVB | 803 (67.7) | 90.4 | 6 [3–10] | 19.9* | 24.2 |
| Total | 1,186 | 85.2 | 6 [3–10] | 17.3 | 23.3 |
*, P<0.001.
Incidence and risk factors of unplanned care
CIF for consultation in the ED and for unplanned hospitalization admission at 12 months after the first evaluation in medical oncology was 71.3% (95% CI: 67.8–74.5%) and 56.7% (95% CI: 53–60%), respectively. The analysis of the time from the first consultation to the event according to grouped stages is shown in Figure 4: CIF of time until 1st consultation in the ED in Figure 4A, and CIF of time until 1st unplanned admission in Figure 4B. For the ED visit, the CIF at 12 months after the first consultation in medical oncology was 50%, 70% and 76% for the grouped stages IA–IIB, IIIA–IIIC and IVA–IVB, respectively. For unplanned admission, the CIF in the same period was 27%, 48% and 66% according to the same grouped stages.
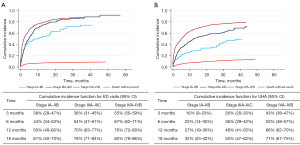
To evaluate factors associated with time to event, the variables stage, ECOG PS, age, sex, histology, smoking, drugs used (steroids, opioids, antibiotics, and anticoagulants), and symptoms in the first assessment (pain, dyspnea, cough, weight loss, and neurologic) were included in a multivariable model. An association was found between the risk of consultation in the ED and the grouped tumor stage, with an increased risk for stages IIIA–IIIC, SHR 1.38, and for stages IVA–IVB, SHR 1.69, compared to stages IA–IIB. No association was observed with the rest of the variables for the ED consultation event. An association was found between unplanned admission and the variables tumor stage, ECOG PS, sex, use of opioids and use of steroids at diagnosis. We observed an increased risk of unplanned admission for stages IIIA–IIIC, SHR 1.64, and stages IVA–IVB, SHR 2.00, both compared to stages IA–IIB. The risk was also increased in ECOG PS 2 patients compared to ECOG PS 0, SHR 1.88; males compared to females, SHR 1.25; opioid use, SHR 1.34, and steroid use, SHR 1.32. The multivariable analysis for ED consultation and unplanned admission is described in detail in Table 3.
Table 3
| Variables included in the analysis | Emergency department visit | Unplanned hospital admission | |||||
|---|---|---|---|---|---|---|---|
| SHR | 95% CI | P | SHR | 95% CI | P | ||
| Stage | |||||||
| IA–IIB | Reference | – | – | Reference | – | – | |
| IIIA–IIIC | 1.38 | 1.03–1.84 | 0.030 | 1.64 | 1.14–2.36 | 0.008 | |
| IVA–IVB | 1.69 | 1.26–2.25 | <0.001 | 2.00 | 1.41–2.85 | <0.001 | |
| ECOG PS | |||||||
| 0 | Reference | – | – | Reference | – | – | |
| 1 | 1.03 | 0.84–1.27 | 0.752 | 1.05 | 0.83–1.33 | 0.706 | |
| 2 | 1.28 | 0.95–1.71 | 0.101 | 1.88 | 1.39–2.53 | <0.001 | |
| 3 | 0.71 | 0.45–1.10 | 0.125 | 1.34 | 0.85–2.11 | 0.205 | |
| 4 | 0.30 | 0.08–1.10 | 0.070 | 1.02 | 0.33–3.15 | 0.04 | |
| Age | |||||||
| <50 years | Reference | – | – | Reference | – | – | |
| 50–64 years | 1.28 | 0.88–1.86 | 0.196 | 1.27 | 0.84–1.93 | 0.253 | |
| 65–74 years | 1.35 | 0.92–1.98 | 0.127 | 1.30 | 0.85–1.98 | 0.219 | |
| ≥75 years | 1.25 | 0.82–1.89 | 0.305 | 1.11 | 0.71–1.74 | 0.650 | |
| Sex | |||||||
| Female | Reference | – | – | Reference | – | – | |
| Male | 1.13 | 0.95–1.36 | 0.171 | 1.25 | 1.02–1.54 | 0.035 | |
| Histology | |||||||
| NSCLC | Reference | – | – | Reference | – | – | |
| SCLC | 1.11 | 0.92–1.35 | 0.279 | 1.06 | 0.84–1.34 | 0.633 | |
| Tobacco use | |||||||
| Non smoker | Reference | – | – | Reference | – | – | |
| Former smoker | 1.11 | 0.80–1.54 | 0.518 | 1.41 | 0.95–2.09 | 0.090 | |
| Active smoker | 1.15 | 0.84–1.58 | 0.368 | 1.44 | 0.97–2.13 | 0.070 | |
| Drug use | |||||||
| No drug use | Reference | – | – | Reference | – | – | |
| Opioids use | 1.10 | 0.88–1.36 | 0.416 | 1.34 | 1.05–1.71 | 0.017 | |
| Steroids use | 1.06 | 0.85–1.32 | 0.630 | 1.32 | 1.04–1.67 | 0.023 | |
| Symptoms | |||||||
| No symptom present | Reference | – | – | Reference | – | – | |
| Cough | 0.99 | 0.84–1.18 | 0.986 | 0.95 | 0.79–1.15 | 0.604 | |
| Dyspnoea | 1.12 | 0.92–1.35 | 0.255 | 1.21 | 0.99–1.49 | 0.068 | |
| Pain | 1.20 | 0.99–1.45 | 0.062 | 1.16 | 0.93–1.43 | 0.181 | |
SHR, subhazard ratio; ECOG PS, Eastern Cooperative Oncology Group Performance Status; NSCLC, non-small cell lung cancer; SCLC, small cell lung cancer.
Discussion
Our study shows that unplanned care for lung cancer patients after the first consultation in a medical oncology department is a very frequent event, with 82.9% of patients requiring consultation in the ED and 68% having an unplanned hospital admission. Unplanned care is, in addition to frequent, an early event for patients with lung cancer, with a 1-year cumulative incidence of 71.3% and 56.7% for ED consultation and for unplanned hospitalization admission, being cancer-related in more than 80% of those episodes. A higher stage increased the risk of ED consultation, while a higher stage, male sex, ECOG PS 2 and treatment with opioids or steroids in the first consultation increased the risk of unplanned admission.
Evaluating patterns of care (23) and identifying patients with a high risk of unplanned medical attention have been suggested as key steps to reduce acute care in cancer patients (14). An approach to the problem has been the evaluation of the burden of emergencies using data from population and administrative registries, reporting between 2.4% and 5.5% of consultations related to cancer out of all emergencies (9-11,24,25), with lung cancer being one of the top three most prevalent primary cancers assigned to cancer-related episodes (9,11,24). Cancer-related attendances had a higher level of acuity, requiring longer management time and length of stay in ED (9), and a significantly higher hospital admission rate: 28.8–90% (9-11,24).
To adapt cancer process management, measuring acute care burden is not enough, and research should also focus on knowing the risk of unplanned care. Lash et al. observed a 44% incidence of ED visits in the Californian population in the year after cancer diagnosis, with a hospitalization rate of 51%. In the lung cancer subgroup, the incidence for ED was 63.8%, being the third neoplasm with the highest risk of ED consultation (26). Our results show a higher 1-year incidence, 71.3%, probably due to a higher proportion of stage IV patients, 63.7%, compared to 17.9% in the Lash et al. study. Despite our higher incidence of ED consultation, a lower hospital admission rate was observed, 42.2% versus 59% for lung cancer patients included in the study by Lash et al., which should justify exploring differences in access to continuity of outpatient care. Similar results were observed in an Australian cohort, with an incidence of ED visits in the first year after diagnosis of 44% in lung cancer patients and a 67% hospitalization rate, being the third neoplasia in emergency consultation risk (27). Both studies used large administrative data, and risks of bias and limitation in the identification of cases should be considered (28), while the results are closer to ours when studying a limited health area, as reported by Hong et al., observing a 57.7% incidence of ED consultation in the first 6 months after diagnosis and 55% in our patients at the same time at risk, with a hospitalization rate of 50.4% (29). ED visits have also been assessed in relation to systemic treatment, with a 45% risk in the 28 days following any treatment in the total population, with a significantly increased incidence for lung cancer patients (30).
When evaluating hospitalizations, Whitney et al. reported an incidence of admission in the first year after diagnosis of advanced cancer of 71% using the California Cancer Registry, with lung cancer being the second neoplasm with the highest risk of admission and readmission (8). Subsequently, they evaluated unplanned hospitalization admission (excluding admissions for chemotherapy, radiotherapy or planned surgery) in patients with cancer, 10.3% lung cancer, observing an incidence of unplanned admission in the year following diagnosis of 35%, but with significant differences between neoplasms, ranging from 14.7% to 57.9%, 55% for lung cancer, very similar to our observation of 56.7% (31). Prince et al. assessed the risk of hospitalization in metastatic non-small cell lung cancer (mNSCLC) during systemic treatment using a meta-analysis of observational studies and randomized clinical trials (RCTs). The admission rate among real-world patients with mNSCLC receiving chemotherapy was significantly higher than that among RCTs, 51% vs. 16%, highlighting the value of real-world studies given the greater selection of patients in RCTs (17). We also observed a 30-day readmission rate of 23.3%, showing that many patients would have a high demand for hospital care, consistent with other reports (32,33).
Regarding potential conditioning factors of unplanned care, in studies based on population and administrative registries, in addition to the association of the risk of emergency consultation with tumor stage, an association was observed with socioeconomic level, age and marital status (26,27), although the limitation of these studies to access individual clinical information on patients should be considered. Assessing unplanned hospitalization, a higher risk of admission has been described for patients with lung cancer, and consistent with our results, an increase in hospitalization has been observed in patients with advanced-stage cancer (31,34), as well as lower socioeconomic status (31) or living alone (34). In the meta-analysis by Prince et al, four of five RCTs and two of five observational studies evaluated factors related to hospitalization, finding that poor performance status in RCTs and chemotherapy regimens received in both types of studies were significantly associated with hospitalization (17). There is controversy among studies regarding the observed higher risk of admission in men, although there is known evidence of differences in patterns of medical care consumption based on sex also in lung cancer (35).
Consultation in ED and unplanned hospitalization admission are related needs but with different incidence and determinants; however, the studies that address both together are limited and very heterogeneous (16). Our study showed that patients with lung cancer have a high need for acute and hospital care, this demand being related to cancer or its treatment in most cases, 86% of visits to the ED and 80% of admissions, so they should be considered in planning and management of medical oncology departments. The management of an oncology service must offer channels and fast tracks for unplanned care, considering the use of strategies and devices for remote monitoring adapted to the risk of each patient and guided by patient-reported outcomes (36-38).
Regarding unplanned outpatient care, 82.9% of patients visited the ED, and the hospitalization rate was 42.2%. The difference identifies consultations that could be attended in another route, being possible to identify the severity of consultations, the attention and resolution time according to the severity, and finally observing the proportion of patients who are discharged after hours in an ED, as shown in Figure 3, all together pointing out the needs of cancer patients and supporting the development of Oncology-Dedicated Emergency Services (39,40). The unplanned hospitalization admission results suggest the possibility of identifying patients at higher risk, especially those with more advanced and symptomatic disease, pointing out the known importance of home care and palliative care interventions (41-44). We highlight the unplanned admission in stage IV, with 43% in the first 3 months, suggesting that the time to demonstrate the usefulness of an intervention for that outcome does not have to be long.
This study has several strengths. The first one included all consecutive lung cancer patients diagnosed at our hospital for 5 years. Given that in Spain health coverage is universal, our patients are fully representative of the general population, avoiding any selection bias. The long recruitment time also increased our sample size, and finally, we think that the recency of recruitment means that we can represent what is currently happening with other lung cancer patients assuming the same healthcare model.
Regarding the shortcomings, the retrospective observational design of the study could mean that some clinical variables influencing unplanned care could be missed, limiting further conclusions about potential factors influencing emergencies and admissions. This study was conducted at a single site, and care resources and process design from our health area may be different from other health systems and therefore not generalizable.
Conclusions
Knowing the risk and burden of unplanned care is key to understanding the needs of patients across the lung cancer care process. Our study shows that lung cancer patients have an extremely high demand for unplanned care, which is an unresolved need. In addition, it is an early need and related to cancer or its treatment in the majority of consultations and admissions and therefore an important issue for the management of medical oncology departments.
Unplanned care is unpredictable but measurable, and metrics represents a key step to quality improvement of health systems. Once the problem has been assessed, the necessary changes must be applied to achieve a true transformation and improvement of care. We must optimize the follow-up of patients with a higher risk of unplanned care, advanced lung cancer, symptomatic or with functional deterioration patients, incorporating remote monitoring strategies which allows for early interventions, as developing specific urgent care pathways for a better comprehensive cancer care.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-23-48/rc
Data Sharing Statement: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-23-48/dss
Peer Review File: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-23-48/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-23-48/coif). MP serves as an unpaid editorial board member of Translational Lung Cancer Research from October 2021 to September 2023. The other authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Cruz-Bermúdez JL, Parejo C, Martínez-Ruíz F, et al. Applying Data Science methods and tools to unveil healthcare use of lung cancer patients in a teaching hospital in Spain. Clin Transl Oncol 2019;21:1472-81. [Crossref] [PubMed]
- Shelburne N, Simonds NI, Jensen RE, et al. Cancer-related emergency and urgent care: expanding the research agenda. Emerg Cancer Care 2022;1:4. [Crossref] [PubMed]
- Cuppens K, Oyen C, Derweduwen A, et al. Characteristics and outcome of unplanned hospital admissions in patients with lung cancer: a longitudinal tertiary center study. Towards a strategy to reduce the burden. Support Care Cancer 2016;24:2827-35. [Crossref] [PubMed]
- Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin 2023;73:17-48. [Crossref] [PubMed]
- Meert AP, Sculier JP, Berghmans T. Lung cancer diagnosis in the emergency department. Eur Respir J 2015;45:867-8. [Crossref] [PubMed]
- Haque N, Raza A, McGoey R, et al. Small cell lung cancer: time to diagnosis and treatment. South Med J 2012;105:418-23. [Crossref] [PubMed]
- Whitney RL, Bell JF, Tancredi DJ, et al. Hospitalization Rates and Predictors of Rehospitalization Among Individuals With Advanced Cancer in the Year After Diagnosis. J Clin Oncol 2017;35:3610-7. [Crossref] [PubMed]
- van der Meer DM, Weiland TJ, Philip J, et al. Presentation patterns and outcomes of patients with cancer accessing care in emergency departments in Victoria, Australia. Support Care Cancer 2016;24:1251-60. [Crossref] [PubMed]
- Hsu J, Donnelly JP, Moore JX, et al. National characteristics of Emergency Department visits by patients with cancer in the United States. Am J Emerg Med 2018;36:2038-43. [Crossref] [PubMed]
- Min HS, Chang HJ, Sung HK. Emergency Department Utilization of Adult Cancer Patient in Korea: A Nationwide Population-Based Study, 2017-2019. Cancer Res Treat 2022;54:680-9. [Crossref] [PubMed]
- Brooks GA, Li L, Uno H, et al. Acute hospital care is the chief driver of regional spending variation in Medicare patients with advanced cancer. Health Aff (Millwood) 2014;33:1793-800. [Crossref] [PubMed]
- Luengo-Fernandez R, Leal J, Gray A, et al. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol 2013;14:1165-74. [Crossref] [PubMed]
- Handley NR, Schuchter LM, Bekelman JE. Best Practices for Reducing Unplanned Acute Care for Patients With Cancer. J Oncol Pract 2018;14:306-13. [Crossref] [PubMed]
- Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006.
- Prince RM, Powis M, Zer A, et al. Hospitalisations and emergency department visits in cancer patients receiving systemic therapy: Systematic review and meta-analysis. Eur J Cancer Care (Engl) 2019;28:e12909. [Crossref] [PubMed]
- Prince RM, Atenafu EG, Krzyzanowska MK. Hospitalizations During Systemic Therapy for Metastatic Lung Cancer: A Systematic Review of Real World vs Clinical Trial Outcomes. JAMA Oncol 2015;1:1333-9. [Crossref] [PubMed]
- Waddle MR, Chen RC, Arastu NH, et al. Unanticipated hospital admissions during or soon after radiation therapy: Incidence and predictive factors. Pract Radiat Oncol 2015;5:e245-53. [Crossref] [PubMed]
- Brooks GA, Uno H, Aiello Bowles EJ, et al. Hospitalization Risk During Chemotherapy for Advanced Cancer: Development and Validation of Risk Stratification Models Using Real-World Data. JCO Clin Cancer Inform 2019;3:1-10. [Crossref] [PubMed]
- Booth CM, Karim S, Mackillop WJ. Real-world data: towards achieving the achievable in cancer care. Nat Rev Clin Oncol 2019;16:312-25. [Crossref] [PubMed]
- Zachariasse JM, van der Hagen V, Seiger N, et al. Performance of triage systems in emergency care: a systematic review and meta-analysis. BMJ Open 2019;9:e026471. [Crossref] [PubMed]
- Austin PC, Fine JP. Practical recommendations for reporting Fine-Gray model analyses for competing risk data. Stat Med 2017;36:4391-400. [Crossref] [PubMed]
- Adelson KB, Velji S, Patel K, et al. Preparing for Value-Based Payment: A Stepwise Approach for Cancer Centers. J Oncol Pract 2016;12:e924-32. [Crossref] [PubMed]
- Rivera DR, Gallicchio L, Brown J, et al. Trends in Adult Cancer-Related Emergency Department Utilization: An Analysis of Data From the Nationwide Emergency Department Sample. JAMA Oncol 2017;3:e172450. [Crossref] [PubMed]
- Peyrony O, Fontaine JP, Beaune S, et al. EPICANCER-Cancer Patients Presenting to the Emergency Departments in France: A Prospective Nationwide Study. J Clin Med 2020;9:1505. [Crossref] [PubMed]
- Lash RS, Bell JF, Bold RJ, et al. Emergency department use by recently diagnosed cancer patients in California. J Community Support Oncol 2017;15:95-102. [Crossref] [PubMed]
- Bureau of Health Information. The Insights Series: Emergency department utilisation by people with cancer. Sydney (NSW); BHI; 2014.
- Msaouel P. The Big Data Paradox in Clinical Practice. Cancer Invest 2022;40:567-76. [Crossref] [PubMed]
- Hong AS, Sadeghi N, Harvey V, et al. Characteristics of Emergency Department Visits and Select Predictors of Hospitalization for Adults With Newly Diagnosed Cancer in a Safety-Net Health System. J Oncol Pract 2019;15:e490-500. [Crossref] [PubMed]
- Dufton PH, Drosdowsky A, Gerdtz MF, et al. Socio-demographic and disease related characteristics associated with unplanned emergency department visits by cancer patients: a retrospective cohort study. BMC Health Serv Res 2019;19:647. [Crossref] [PubMed]
- Whitney RL, Bell JF, Tancredi DJ, et al. Unplanned Hospitalization Among Individuals With Cancer in the Year After Diagnosis. J Oncol Pract 2019;15:e20-9. [Crossref] [PubMed]
- Montero AJ, Stevenson J, Guthrie AE, et al. Reducing Unplanned Medical Oncology Readmissions by Improving Outpatient Care Transitions: A Process Improvement Project at the Cleveland Clinic. J Oncol Pract 2016;12:e594-602. [Crossref] [PubMed]
- Guven DC, Ceylan F, Cakir IY, et al. Evaluation of early unplanned readmissions and predisposing factors in an oncology clinic. Support Care Cancer 2021;29:4159-64. [Crossref] [PubMed]
- Ullgren H, Sharp L, Olofsson A, et al. Factors associated with healthcare utilisation during first year after cancer diagnose-a population-based study. Eur J Cancer Care (Engl) 2021;30:e13361. [Crossref] [PubMed]
- Rana RH, Alam F, Alam K, et al. Gender-specific differences in care-seeking behaviour among lung cancer patients: a systematic review. J Cancer Res Clin Oncol 2020;146:1169-96. [Crossref] [PubMed]
- Simon BA, Assel MJ, Tin AL, et al. Association Between Electronic Patient Symptom Reporting With Alerts and Potentially Avoidable Urgent Care Visits After Ambulatory Cancer Surgery. JAMA Surg 2021;156:740-6. [Crossref] [PubMed]
- Daly B, Nicholas K, Flynn J, et al. Analysis of a Remote Monitoring Program for Symptoms Among Adults With Cancer Receiving Antineoplastic Therapy. JAMA Netw Open 2022;5:e221078. [Crossref] [PubMed]
- Offodile AC 2nd, DiBrito SR, Finder JP, et al. Active surveillance of chemotherapy-related symptom burden in ambulatory cancer patients via the implementation of electronic patient-reported outcomes and sensor-enabled vital signs capture: protocol for a decentralised feasibility pilot study. BMJ Open 2022;12:e057693. [Crossref] [PubMed]
- Turgeman I, Bar-Sela G. Effective Patient Selection for an Oncology-Dedicated Emergency Service: A Retrospective Study. JCO Oncol Pract 2021;17:e1567-75. [Crossref] [PubMed]
- Gould Rothberg BE, Canavan ME, Mun S, et al. Impact of a Dedicated Cancer Urgent Care Center on Acute Care Utilization. JCO Oncol Pract 2022;18:e129-36. [Crossref] [PubMed]
- Obermeyer Z, Makar M, Abujaber S, et al. Association between the Medicare hospice benefit and health care utilization and costs for patients with poor-prognosis cancer. JAMA 2014;312:1888-96. [Crossref] [PubMed]
- Sanchez JC, Gomez-Bravo R, Morito Aguilar AM, et al. Palliative care in advanced cancer: A clinical and ethical goal achieved? Ann Oncol 2018;29:VIII552.
- Mooney K, Titchener K, Haaland B, et al. Evaluation of Oncology Hospital at Home: Unplanned Health Care Utilization and Costs in the Huntsman at Home Real-World Trial. J Clin Oncol 2021;39:2586-93. [Crossref] [PubMed]
- Gamblin V, Prod'homme C, Lecoeuvre A, et al. Home hospitalization for palliative cancer care: factors associated with unplanned hospital admissions and death in hospital. BMC Palliat Care 2021;20:24. [Crossref] [PubMed]


