
Non-bacterial thrombotic endocarditis in ROS1-rearranged lung cancer: a report of two cases
Highlight box
Key findings
• Patients with ROS1-rearranged lung adenocarcinoma are at higher risk of developing non-bacterial thrombotic endocarditis (NBTE), which can lead to neurological symptoms, and early initiation of oncologic treatment along with anticoagulation may improve neurological symptoms and antitumor response.
What is known and what is new
• Lung cancer, especially adenocarcinoma, is associated with a high incidence of thromboembolic events including NBTE, with higher risk in patients with ALK and ROS1 rearrangements. EGFR mutation is also related to such thrombotic complication, although less frequently.
• This study presents two cases of ROS1-rearranged lung adenocarcinoma with NBTE, highlighting the potential benefit of early oncologic treatment initiation upon NBTE diagnosis, leading to improved neurological symptoms and antitumor response.
What is the implication and what should change now?
• The findings emphasize the need for early recognition, interdisciplinary collaboration, and prompt initiation of oncologic treatment with anticoagulation in patients with ROS1-rearranged lung adenocarcinoma and NBTE to improve outcomes.
Introduction
Background
Lung cancer is associated with high incidence of thromboembolic events (TE). Up to 15% of patients with advanced lung adenocarcinoma will present a TE (1,2). Patients with ALK and ROS1 rearrangements have been identified as a population of higher risk of TE. One severe form of TE is non-bacterial thrombotic endocarditis (NBTE), defined as the presence of sterile vegetations on cardiac valves that can cause organ damage by cardioembolic mechanism. It is very infrequent though with an estimated overall incidence between 0.9% and 1.6% in autopsy populations (3). Malignancy is the most frequent cause of NBTE, causing up to 75% of cases, and being lung cancer the most prevailing malignant cause (28% of malignant-related NBTE), while the remaining 25% correspond to non-malignant causes (i.e., systemic lupus erythematosus) (3). Medical treatment includes anticancer treatment, anticoagulation with heparin, direct oral anticoagulation (DOAC) or vitamin k antagonists (4). In some cases, surgical approach may be necessary, in a case-by-case basis (if presence of heart failure, big valve vegetations or medical treatment failure with recurrent embolism) (5). Here we report two cases of patients with ROS1-rearranged lung adenocarcinoma who developed NBTE.
Rationale and knowledge gap
NBTE can be a diagnostic challenge and a complex disease to treat. Clinical guidelines show recommendations to diagnosis and treatment, but low frequency of this disease makes it difficult to generate new evidence.
Objective
To describe the clinical presentation of two cases of NBTE associated to ROS1 positive lung cancer and to bring new evidence of the clinical benefit of initiating oncologic treatment as soon as the diagnosis of NBTE is made. We present these cases in accordance with the CARE reporting checklist (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-23-412/rc).
Case presentation
Case 1
A 42-year-old never smoker Caucasian woman without past medical history, two healthy children and no history of abortions, was diagnosed in January 2022 of a stage IV lung adenocarcinoma with an isolated brain metastasis and ROS1 rearrangement, T1N2M1c. She was treated with stereotactic body radiation therapy (30 Gy in 3 fractions) for the brain metastasis and was then included in a clinical trial where she received treatment with crizotinib. Right after beginning treatment, she was diagnosed of pulmonary embolism (PE) and deep vein thrombosis (DVT) of the lower right limb, receiving anticoagulation with low molecular weight heparin that was maintained per recommendation of Vascular medicine department. She responded to crizotinib with a partial response for 7 months assessed by brain magnetic resonance imaging (MRI) and computed tomography (CT) scan of chest and abdomen, with good tolerability. At this point, she was diagnosed with a symptomatic cerebral progression in the form of multiple small metastases. She had to interrupt heparin because of an asymptomatic hemorrhage found on brain MRI. She received whole brain radiation and was planned to begin second-line treatment with lorlatinib on September 2022.
Days before the appointment to initiate treatment, on 09/09/2022, the patient was admitted to the emergency room with acute loss of movement of left upper and lower limbs and seizures. Her Glasgow score was 15. A CT scan was performed revealing brain metastases increased in number and edema. She was started on corticosteroids and anticonvulsive drugs.
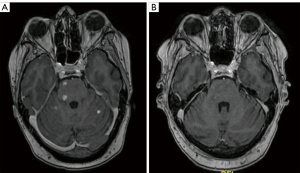
Initial blood tests showed low platelet count, low fibrine, high d-dimer and coagulation times, being diagnosed of Disseminated Intravascular Coagulation (DIC). In the next hours the patient presented a neurological worsening with Glasgow score of 10. Management by the Intensive Care Unit was required to protect the airway, remaining hemodynamically stable, with persistent neurologic worsening. Brain MRI showed multiple ischemic brain lesions not seen on the CT scan, consistent with cardioembolic disease (Figure 1).

With the suspicion of NBTE, a transthoracic echocardiography (TTE) was performed on 09/12/2023 that confirmed the presence of a cardiac vegetation on the mitral valve. After ruling out infective endocarditis with negative blood cultures, she was finally diagnosed of NBTE with associated DIC. Due to thrombocytopenia, low-weight molecule heparin (LWMH) at a medium dose (40 mg enoxaparin/day) was started. Being under anticoagulation treatment, the patient presented another cardioembolic accident with secondary tetraplegia, dysphagia and clinical deterioration.
Lorlatinib was initiated in crushed form in a dilution through a nasogastric tube on 09/14/2023. Normalization of blood test values and partial neurological improvement were achieved by 09/19/2023. No new TEs developed and the patient progressively improved her neurological symptoms, with resolution of tetraplegia (with a gain in motor function of the four limbs, being able to walk with help), improving the level of consciousness to Glasgow 15 and with partial resolution of aphasia. Objective response to lorlatinib was confirmed in the brain the 12/13/2022, by MRI (Figure 2). She presented in September 2023 brain progression treated with focal radiotherapy (total dose 20 Gy) and continued on lorlatinib treatment. In October 2023, the patient was currently able to talk, walk with a stick and eat normally, with correct tolerability to treatment.
Case 2
A Black 54-year-old man, active smoker with 55 packs-year burden and with history of hypertension was admitted in the emergency room on September 2022 presenting left hemiparesis and numbness. He was diagnosed of a capsule-thalamus stroke by contrast enhanced CT scan of the brain. Atrial fibrillation was ruled out by electrocardiogram. He was prescribed aspirin and was discharged after 48-hour observation, with vital signs on range. Three weeks later, on 10/14/2022, he consults the emergency department for cervical palpable mass. In the physical exam he presented palpable lateral cervical lymphadenopathy. Interrogating the patient, he explained mild hemoptysis. After a complete diagnostic work up, he was diagnosed on November 2022 of a stage IV lung adenocarcinoma, T4N3M1c with contralateral lung, bone and multiple lymph nodes metastasis.
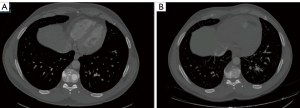
The patient reconsulted the emergency service on 11/11/2022, two days after the cancer diagnosis was made and two months after the first emergency department consultation, presenting dysesthesia and paresthesia of the right arm. At initial assessment his vital signs were on range, his Eastern Cooperative Oncology Group Performance Status (ECOG PS) was 1 and showed no other symptoms. The neurological physical exam showed hypoesthesia in the right upper and lower limbs with no motor deficits. Blood tests showed elevated alkaline phosphatase (grade 2) and mild anemia (grade 1). A brain CT scan was performed showing a larger ischemic area of the known thalamic involvement and new ischemic images in the parietal area of the brain. He was hospitalized to continue the diagnostic work up and establish treatment. A brain MRI showed numerous bilateral subacute and chronic ischemic lesions at the parietal and periventricular subcortical levels not observed on the CT scan (Figure 3). To rule out a cardioembolic mechanism, a TTE was performed, showing no significant results. However, the transesophageal echocardiography (TEE) revealed an aortic valve vegetation. Along with negative blood cultures, the diagnosis of NBTE was confirmed. No ultrasound was performed to rule out DVT of limbs, but the chest CT scan ruled out pulmonary emboli. LWMH was initiated and the patient was discharged the next 48 hours. Molecular studies of the lung adenocarcinoma revealed a ROS1 rearrangement. Therefore, the patient started on crizotinib 250 mg/12 h hours orally as first line treatment, presenting radiologic partial response on November 2022 (Figure 4) with no toxicity. The patient remains on treatment with improvement of neurological symptoms. Due to persistent grade 2 neutropenia, the patient needed dose reduction of crizotinib to 200 mg/12 h, but on October 2023 the patients kept on good performance status and no signs of progression.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Verbal informed consent has been obtained from the patients before the making of this manuscript.
Discussion
Patients harboring ROS1-rearranged advanced lung cancer are reported to present more TE of any kind and most of the events occur within the 90-day peri-diagnostic window (1).
TE can be associated with poor prognosis and shortened progression-free survival in lung cancer patients (6). Specifically, when analyzing patients diagnosed of NBTE, the subpopulation presenting lung cancer show higher mortality in 1 year than patients with other malignant underlying conditions (7).
NBTE is a thrombotic paraneoplastic phenomenon characterized by sterile thrombotic friable cardiac vegetations composed of fibrin and platelet aggregates. Its pathophysiological origin involves endothelial damage, hypercoagulability and circulating immunocomplexes (8). Cancer is the most frequent underlying cause, mostly adenocarcinoma of lung and ovary, that produce mucin as a procoagulant factor. ROS1 rearrangements may confer an increased hypercoagulability state through its downstream signaling activation, creating cross-talk with procoagulant factors like tissue factor, thus triggering subsequent thrombin formation (6).
To reach the diagnosis of NBTE, clinical suspicion is key when assessing patients with embolic symptoms. Patients can present neurological focality as impaired level of consciousness, motor or sensitive deficits of a limb and they can show cutaneous involvement such as skin necrosis, all of them signs and symptoms caused by a cardioembolic mechanism.
In the diagnostic work-up, TTE is usually performed first due to its wide availability, non-invasive nature, and ability to better visualize valvular lesions on the tricuspid valve. TEE has higher sensitivity than TTE in patients with smaller lesions, morbid obesity, abscesses, new atrioventricular block, chronic obstructive lung disease and especially in patients with prosthetic valves (5). It is necessary to rule out infective endocarditis by the modified Duke criteria. Infectious endocarditis should be considered when presenting two major diagnostic criteria like microorganism identification on 2 or more separate blood cultures, vegetation seen on cardiac valve through echocardiogram or abnormal metabolic activity on cardiac valve on positron emission tomography-CT (PET-CT), or presenting multiple minor criteria like documented fever, documented cerebral or splenic abscess, immunologic phenomena like Osler nodes or positive rheumatoid factor (9).
Optimal therapy of NBTE includes anticoagulation and treatment of the underlying condition, in these cases being the treatment targeting the ROS1 rearrangement. Unfractionated heparin, LMWH and warfarin can decrease the risk of embolization and thrombotic recurrence, though some studies suggest more efficacy from heparin than vitamin k inhibitors reducing the risk of recurrent thrombosis (4). There is no definite evidence demonstrating the efficacy of fondaparinux. Direct oral anticoagulants as rivaroxaban, apixaban or edoxaban are equally acceptable alternatives but should be used carefully in patients with gastrointestinal or genitourinary tracts tumors, due to the considerable risk of bleeding events (4).
Indications for valvular repair or replacement include heart failure due to severe valvular dysfunction, new heart block, large vegetations greater than 1 cm, or recurrent embolism despite optimal medical management (5).
Both our patients started showing neurological symptoms, but without skin involvement. One of them required TEE because the TTE showed no cardiac valve vegetation. Both of them were hospitalized, received heparin and oncologic targeted treatment with tyrosine-kinase inhibitors (TKI), one with second-line lorlatinib, the other with first-line crizotinib, and they both showed improvement of neurological symptoms associated with antitumor response. One of them needed assessment of the Intensive Care Unit team because of severe neurological symptoms, and presented great neurological improvement the weeks after initiating targeted treatment with, being able to walk with a stick and to have simple conversations, with just residual bradylalia. This case emphasizes the need to establish early antitumoral treatment due to potential Lazarus effect (10) expected from these highly active drugs, as seen in our patient.
Patients with advanced lung cancer are at higher risk of thrombotic events and this risk is increased in patients whose tumors harbor ALK and ROS1 alterations. Neurological TE may have a great impact in patients’ quality of life and should be diagnosed and treated promptly. Prophylactic anticoagulation has not demonstrated a clear impact in survival (4) but patients with uncontrolled disease, that are at greater risk, should be closely monitored and early suspicion should arise at first symptoms. In patients at low risk of bleeding events, prophylactic heparin or direct oral anticoagulants might be considered keeping close monitoring of bleeding events and always taking into account the risk-benefit balance in a case-by-case basis (4).
This report highlights the importance of initial clinical suspicion of NBTE to make a prompt diagnosis, in order to obtain good clinical outcomes from directed oncological treatment. Despite that, one of our patients presented initial neurological worsening even receiving optimal treatment, due to the aggressiveness of this disease, as seen in some reports 79% of patients can have an embolic event 1 month after the NBTE diagnosis (7) and being the 3-month estimated overall survival of 26% of patients diagnosed of lung cancer induced NBTE (3). The main limitation of our report is the possible selection bias of our patients as we are reporting two cases with great improvement after treatment.
Conclusions
NBTE is a rare and severe thrombotic event associated with advanced malignancy, showing neurologic and dermatologic symptomatology. Clinical suspicion and fast diagnosis in patients with neoplasms with high risk such as ROS1-rearranged lung cancer are the key to improve prognosis of these patients, requiring anticoagulation and treating the underlaying cancer as soon as possible.
Acknowledgments
Funding: This study was funded by
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-23-412/rc
Peer Review File: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-23-412/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-23-412/coif). J.R.B. reports travel support from Adamed and LEO Pharma, outside the submitted work. P.R. reports travel support from AstraZeneca, MSD, BMS, and Kiowa Kirin, outside the submitted work. A.T. reports consulting fees from Sanofi; payment or honoraria from Roche, Pfizer, BMS, GSK, AZ, and MSD; and support for attending meetings from GSK, and AZ. E.A. reports receiving consulting fees as a consultant or advisory role in MSD, Bristol-Myers, Roche, Boehringer Ingelheim, Pfizer, Novartis, AstraZeneca, Lilly, and Takeda; speaking fees from MSD, Bristol-Myers, Roche, Boehringer Ingelheim, Pfizer, Novartis, AstraZeneca, Lilly, and Takeda; he is also a co-founder of Trialing Health S.L. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Verbal informed consent has been obtained from the patients before the making of this manuscript.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ng TL, Smith DE, Mushtaq R, et al. ROS1 Gene Rearrangements Are Associated With an Elevated Risk of Peridiagnosis Thromboembolic Events. J Thorac Oncol 2019;14:596-605. [Crossref] [PubMed]
- Ng TL, Tsui DCC, Wang S, et al. Association of anticoagulant use with clinical outcomes from crizotinib in ALK- and ROS1-rearranged advanced non-small cell lung cancers: A retrospective analysis of PROFILE 1001. Cancer Med 2022;11:4422-9. [Crossref] [PubMed]
- Rahouma M, Khairallah S, Dabsha A, et al. Lung Cancer as a Leading Cause among Paraneoplastic Non-Bacterial Thrombotic Endocarditis: A Meta-Analysis of Individual Patients' Data. Cancers (Basel) 2023;15:1848. [Crossref] [PubMed]
- Lyman GH, Carrier M, Ay C, et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv. 2021;5(4):927-974. Blood Adv 2021;5:1953. [Crossref] [PubMed]
- Liu J, Frishman WH. Nonbacterial Thrombotic Endocarditis: Pathogenesis, Diagnosis, and Management. Cardiol Rev 2016;24:244-7. [Crossref] [PubMed]
- Liu Y, Wang W, Wu F, et al. High discrepancy in thrombotic events in non-small cell lung cancer patients with different genomic alterations. Transl Lung Cancer Res 2021;10:1512-24. [Crossref] [PubMed]
- Quintero-Martinez JA, Hindy JR, El Zein S, et al. Contemporary demographics, diagnostics and outcomes in non-bacterial thrombotic endocarditis. Heart 2022;heartjnl-2022-320970.
- Cheung B, Shivkumar A, Ahmed AS. Embolic Showering from Non-Bacterial Thrombotic Endocarditis and Adenocarcinoma of the Lung. Eur J Case Rep Intern Med 2020;7:001798. [Crossref] [PubMed]
- Fowler VG, Durack DT, Selton-Suty C, et al. The 2023 Duke-International Society for Cardiovascular Infectious Diseases Criteria for Infective Endocarditis: Updating the Modified Duke Criteria. Clin Infect Dis 2023;77:518-26. Erratum in: Clin Infect Dis 2023;77:1222. [Crossref] [PubMed]
- Facchinetti F, Levy A, Ammari S, et al. Meningeal "Lazarus Response" to Lorlatinib in a ROS1-Positive NSCLC Patient Progressing to Entrectinib. Cancer Manag Res 2021;13:2805-10. [Crossref] [PubMed]


