
The potential high-risk population for lung cancer screening: determination of initial screening age and heterogeneity in histology and sex
Highlight box
Key findings
• Patients aged 50 to 54 years can benefit from lung cancer screening.
• The survival benefits may be more apparent in adenocarcinoma.
• Younger male patients may benefit more than female patients.
What is known and what is new?
• Lung cancer screening has been demonstrated that it can significantly reduce mortality rates using low-dose computed tomography.
• Our findings revealed a significant survival advantage for patients aged 50–54 years compared to those aged 55–59 years, particularly pronounced in adenocarcinoma cases. The significant benefits remained among the male patients when the comparison was expanded to 45 years.
What is the implication, and what should change now?
• These results are consistent with the recommendations released by the US Preventive Services Task Force (USPSTF) in 2021 and accurate screening strategies might need to be formulated based on tumor histology and patient sex.
Introduction
Lung cancer remains the primary cause of cancer-related mortality globally (1). Lung cancer screening has been demonstrated that it can significantly reduce mortality rates using low-dose computed tomography (CT) (2). According to the National Lung Screening Trial (NLST), annual low-dose CT scans resulted in a 20% reduction in lung cancer-related deaths compared to chest radiography (3). Similarly, the Nederlands Leuvens Screening Onderzoek (NELSON) confirmed that low-dose CT scans can effectively decrease the lung cancer-related mortality among the potential high-risk populations by 24% (4).
The lung cancer screening criteria for high-risk groups are mainly related to age and smoking history (5). Discrepancy remains regarding the extent of potential high-risk populations based on age considerations for the low-dose CT screening. Individuals aged 55–74 were defined as those at high risk in the NLST (3), which was also supported by the American Cancer Society (ACS) (6) and the American Association for Thoracic Surgery (AATS) (7) of which its recommendations are applied to persons over 55 years of age. However, the US Preventive Services Task Force (USPSTF) expanded these screening criteria to individuals over 50 years of age in 2021, although adults aged 55–80 years were first recommended for annual low-dose CT screening in 2013 (8). Similarly, the National Comprehensive Cancer Network (NCCN) (9) and the American Lung Association (ALA) also consider individuals over the age of 50 years as high-risk populations for low-dose CT scans (10). The American College of Chest Physicians (ACCP) strongly recommends screening for patients aged 55–77, and recommendation is suggested for patients aged 50–80 (11).
Additionally, it has been reported that low-dose CT screening confers distinct survival advantages among different pathological subtypes compared to chest radiography (12,13). Considering a significant increase in the proportion of adenocarcinomas in recent years and a potential effect of sex on the formulation of lung cancer screening strategies (14-17), we speculate heterogeneity in screening strategies across different histologies and sexes.
Therefore, the Surveillance, Epidemiology, and End Results (SEER) database was utilized to explore the potential survival benefits of lung cancer screening among individuals aged 50–54 years and assess heterogeneity based on pathological types and sex. Given that the small cell lung cancer (SCLC) is less prevalent and metastasizes so rapidly that cannot be reliably identified through screening in early-stage detection when it may still be treatable (8), our analysis focused on patients with non-small cell lung cancer (NSCLC). We present this article in accordance with the STROBE reporting checklist (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-475/rc).
Methods
Data source and patient selection
The SEER database is an authoritative resource for cancer statistics supported by the Surveillance Research Program (SRP) in the National Cancer Institute (NCI)’s Division of Cancer Control and Population Sciences (DCCPS). The data cover approximately 48% populations in America, and the cancer statistics are collected at a national level (18).
We included 234,975 patients diagnosed with NSCLC between 2011 and 2016 from SEER 18 registries. Exclusions were made for NSCLC without microscopic confirmation (n=3,632), with a historical diagnosis of other malignancies (n=75,584), reported on autopsy or death certificate only (n=190), and without a definite cause of death (n=1,398). Finally, our analysis included 154,171 patients diagnosed with NSCLC. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Population characteristics
Characteristic information filtered from the SEER database included age (<45, 45–49, 50–54, 55–59, and >59 years), sex, race (White, Black, or other), year of diagnosis, tumor stage (I/II, III, IV, or missing), histology (adenocarcinoma, squamous cell carcinoma, or other NSCLC), surgery, radiation, and chemotherapy. The tumor stage was determined according to the American Joint Committee on Cancer sixth edition [2006–2015] and the SEER stage group [2016]. For patients whose stage information was incomplete, we utilized the SEER historic stage A [1973–2015] for stage assignment. Stage I/II, III, IV were separately defined as those with historic localized, regional, and distant stage values. To assess the tumor stage alteration, we conducted a sensitivity analysis and found that there were no significant alterations in the distribution of tumor stages after the exclusion of data from 2015. NSCLC subtypes were classified based on the International Classification of Diseases for Oncology, 3rd edition (ICD-O-3), and morphology codes (19).
Regarding the inclusion of the age range for further analysis, we evaluated the incidence of lung cancer diagnoses at one-year age intervals throughout the included population and set 80 years as the upper age limit for the comparison of patient coverage proportion based on risk factor-based strategies in a modeling study of the USPSTF recommendations in 2021 (20). Finally, the analysis was initiated for individuals aged >45. Considering the potential differences in biological factors and the possibility of introducing massive mortality events unrelated to lung cancer diagnosis among patients over 60 years of age (21), three age groups (55–59, 50–54 and 45–49 years) were stratified among the study population with a five-year interval, and the adjacent age groups were compared separately (45–49 vs. 50–54 years, and 50–54 vs. 55–59 years), using overall survival (OS) and lung cancer-specific survival (LCSS) as survival outcomes.
Statistical analysis
Descriptive analyses were conducted to examine individual characteristics across different age groups, and the comparison of categorical variables between each pair of groups was conducted by chi-squared tests. The hazard ratios (HRs) and 95% confidence intervals (CIs) for OS and LCSS were calculated by the Cox proportional hazard regression. The following covariates were fully adjusted for modeling as potential predictors of survival: sex, race, stage, histology, surgery, radiation, and chemotherapy. Considering that lung cancer screening might significantly affect the stage, we also modeled the stage separately (22). In addition, we calculated the average annual percentage change (AAPC) in tumor pathological characteristics by Joinpoint software version 4.9.1.0 (National Cancer Institute) based on t-tests. Statistical analyses were performed based on the R statistical software version 4.2.1 (R Project for Statistical Computing). A level of P=0.05 was established for the statistical significance of all analyses performed.
Results
Among the 154,171 patients with NSCLC [81,162 (52.64%) men] between 2011 and 2016, there were 4,203, 10,126, and 17,122 patients aged 45–49, 50–54, and 55–59 years, respectively. Compared to the 50–54 age group, a larger proportion of patients aged 45–49 were another race than Black or White, had adenocarcinoma or other NSCLC, and received chemotherapy. However, female, advanced-stage diagnosis, adenocarcinoma histology, and utilization of radiation therapy and chemotherapy were more common among patients aged 50–54 years than among those aged 55–59 years. Patient information according to the age group is presented in Table 1.
Table 1
| Characteristic | Age group, n (%) | P1 | P2 | ||||
|---|---|---|---|---|---|---|---|
| <45 y (n=2,907) | 45–49 y (n=4,203) | 50–54 y (n=10,126) | 55–59 y (n=17,122) | >59 y (n=119,813) | |||
| Sex | 0.09 | <0.001 | |||||
| Male | 1,378 (47.40) | 2,118 (50.39) | 5,261 (51.96) | 9,432 (55.09) | 62,973 (52.56) | ||
| Female | 1,529 (52.60) | 2,085 (49.61) | 4,865 (48.04) | 7,690 (44.91) | 56,840 (47.44) | ||
| Race | <0.001 | 0.15 | |||||
| White | 2,067 (71.10) | 3,024 (71.95) | 7,447 (73.54) | 12,772 (74.59) | 96,317 (80.39) | ||
| Black | 399 (13.73) | 718 (17.08) | 1,848 (18.25) | 3,015 (17.61) | 13,086 (10.92) | ||
| Other | 441 (15.17) | 461 (10.97) | 831 (8.21) | 1,335 (7.80) | 10,410 (8.69) | ||
| Year of diagnosis | <0.001 | <0.001 | |||||
| 2011 | 540 (18.58) | 853 (20.30) | 1,842 (18.19) | 2,686 (15.69) | 19,258 (16.07) | ||
| 2012 | 474 (16.31) | 796 (18.94) | 1,755 (17.33) | 2,821 (16.48) | 19,457 (16.24) | ||
| 2013 | 488 (16.79) | 694 (16.51) | 1,660 (16.39) | 2,857 (16.69) | 19,667 (16.41) | ||
| 2014 | 477 (16.41) | 660 (15.70) | 1,721 (17.00) | 2,898 (16.93) | 19,973 (16.67) | ||
| 2015 | 476 (16.37) | 632 (15.04) | 1,646 (16.26) | 2,902 (16.95) | 20,498 (17.11) | ||
| 2016 | 452 (15.55) | 568 (13.51) | 1,502 (14.83) | 2,958 (17.28) | 20,960 (17.49) | ||
| Stage | 0.51 | <0.001 | |||||
| I/II | 762 (26.21) | 827 (19.68) | 2,098 (20.72) | 3,935 (22.98) | 33,996 (28.37) | ||
| III | 570 (19.61) | 967 (23.01) | 2,329 (23.00) | 3,983 (23.26) | 28,441 (23.74) | ||
| IV | 1,533 (52.73) | 2,352 (55.96) | 5,555 (54.86) | 8,972 (52.40) | 54,761 (45.71) | ||
| Missing | 42 (1.44) | 57 (1.36) | 144 (1.42) | 232 (1.35) | 2,615 (2.18) | ||
| Histology | <0.001 | <0.001 | |||||
| Adenocarcinoma | 1,720 (59.17) | 2,718 (64.67) | 6,464 (63.84) | 10,412 (60.81) | 66,990 (55.91) | ||
| Squamous cell carcinoma | 277 (9.53) | 647 (15.39) | 1,916 (18.92) | 3,826 (22.35) | 35,117 (29.31) | ||
| Other NSCLC | 910 (31.30) | 838 (19.94) | 1,746 (17.24) | 2,884 (16.84) | 17,706 (14.78) | ||
| Surgery | 0.45 | 0.77 | |||||
| Yes | 1,077 (37.05) | 1,068 (25.41) | 2,511 (24.80) | 4,274 (24.96) | 27,386 (22.86) | ||
| No/unknown | 1,830 (62.95) | 3,135 (74.59) | 7,615 (75.20) | 12,848 (75.04) | 92,427 (77.14) | ||
| Radiation | 0.36 | 0.02 | |||||
| Yes | 1,191 (40.97) | 2,061 (49.04) | 4,878 (48.17) | 7,986 (46.64) | 46,740 (39.01) | ||
| No/unknown | 1,716 (59.03) | 2,142 (50.96) | 5,248 (51.83) | 9,136 (53.36) | 73,073 (60.99) | ||
| Chemotherapy | <0.001 | <0.001 | |||||
| Yes | 1,699 (58.45) | 2,685 (63.88) | 6,101 (60.25) | 9,721 (56.77) | 49,301 (41.15) | ||
| No/unknown | 1,208 (41.55) | 1,518 (36.12) | 4,025 (39.75) | 7,401 (43.23) | 70,512 (58.85) | ||
P1, individuals aged 45–49 years vs. individuals aged 50–54 years; P2, individuals aged 50–54 years vs. individuals aged 55–59 years. NSCLC, non-small cell lung cancer.
Patients aged 55–80 years, representing a potentially high-risk population, constituted 75.01% (115,642 individuals) of the total. By expanding the initial age to 45 and 50 years, the proportion of patients with potentially high risk increased to 81.58% (125,768 individuals) and 84.30% (129,971 individuals), respectively. However, when we expanded the initial age to 40 years, the coverage proportion increased by only 1.02% (Figure S1).
Compared to the patients aged 55–59 years, the unadjusted HRs for OS and LCSS were 0.95 (95% CI: 0.93–0.98) and 0.97 (95% CI: 0.94–1.00) among the patients aged 50–54 years, respectively. Significant differences in OS and LCSS were observed after adjusting for stage [OS: 0.89 (0.87–0.92), LCSS: 0.91 (0.88–0.93)]. Within the fully adjusted model, the HRs for OS and LCSS were finally 0.94 (95% CI: 0.92–0.96) and 0.94 (95% CI: 0.91–0.97) (Figure 1A). For patients aged 45–49 years, the HRs for OS and LCSS were 0.94 (95%, 0.90–0.98) and 0.95 (95% CI: 0.91–0.99) after an adjustment for stage compared with patients aged 50–54 years. However, there was no survival advantage in OS and LCSS [OS: 0.97 (0.93–1.01), LCSS: 0.98 (0.93–1.02)] within the fully adjusted model (Figure 1B).

Significant increases in the proportion of adenocarcinomas were observed in patients aged 45–59 years. Among all included patients (Figure 2), the percentage of individuals with adenocarcinoma increased from 58.99% in 2011 to 65.04% in 2016 (AAPC, 2.2; 95% CI: 1.4–2.9). The observed trends were consistent across all age groups.

Further subgroup analyses were conducted among the different age groups based on histology. For individuals diagnosed with adenocarcinoma, the unadjusted HRs for OS and LCSS were 0.96 (95% CI: 0.93–0.99) and 0.98 (95% CI: 0.94–1.02) comparing 50–54 years group to 55–59 years group, respectively. After adjusting for the tumor stage, the respective HRs for OS and LCSS were 0.90 (95% CI: 0.87–0.94) and 0.92 (95% CI: 0.88–0.95). Within the fully adjusted model, significant differences were still observed in OS and LCSS [OS: 0.93 (0.90–0.97), LCSS: 0.95 (0.91–0.98)] (Figure 3A). There was no significant survival advantage between patients aged 45–49 years and those aged 50–54 years after adjustment (Figure 3B). However, no survival advantage was observed among individuals with squamous cell carcinoma (Figure 3C,3D).
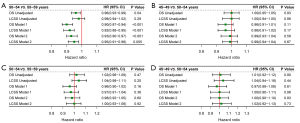
In the subgroup analysis based on patient sex, although no significant survival advantages were observed in the unadjusted model for OS and LCSS [OS: 0.98 (0.95–1.02), LCSS: 1.01 (0.97–1.05)] among the male patients aged 50–54 years compared with those aged 55–59 years, the HRs were 0.92 (95% CI: 0.89–0.96) and 0.94 (95% CI: 0.90–0.98) for OS and LCSS after adjusting for stage. In the fully adjusted model, the HRs were 0.95 (95% CI: 0.91–0.98) and 0.96 (95% CI: 0.93–1.00) for OS and LCSS, respectively (Figure 4A). However, when the comparison was expanded to 45 years, significant benefits remained among the male patients with respective HRs of 0.91 (95% CI: 0.86–0.97) for OS and 0.92 (95% CI: 0.87–0.98) for LCSS in the fully adjusted model (Figure 4B). For female patients aged 50–54 years, significant survival advantages were also observed in the three models compared with female patients aged 55–59 years (Figure 4C). However, similar benefits were not observed between female patients aged 45–49 years and those aged 50–54 years (Figure 4D).

Discussion
This study demonstrated that patients aged 50–54 years can benefit from lung cancer screening, which validates the reliability of the USPSTF guidelines. The survival benefits are probably more apparent in adenocarcinoma. Younger male patients could benefit more than female patients, which may reflect the need for sex differences in cancer screening strategies.
Age plays a crucial role as an inclusion criterion for lung cancer screening. In our study, it was observed that patients aged 50–54 years had a significant survival advantage in both OS and LCSS compared with those aged 55–59 years in the multivariate model based on the SEER database. In contrast, no advantage was observed in initiating screening at age 45. Therefore, our findings support the expansion of lung cancer screening to the initial age of 50 years, consistent with the recommendations released by the USPSTF in 2021. According to the guidelines for lung cancer screening announced by different international associations, 55 years is commonly recommended as the initial age of high-risk groups. This is concordant with the clinical trial results reported by the NLST in 2011 (6,7,23-25). As the largest randomized controlled trial (RCT), the NLST conducted the analysis on individuals aged 55–74 and reported that low-dose CT scans could lead to a 20% reduction in lung cancer mortality (3). However, NELSON expanded the initial age criteria to 50 years, with a significant decrease of 24% in mortality rates associated with lung cancer (4). Combined with these clinical trials and the application of the CISNET model, the USPSTF expanded the age criterion to 50 years by 2021 (8). This expansion of the initial screening age was also supported by the NCCN, ACCP, and ALA based on the current guidelines for lung cancer screening (Table 2). Several modeling studies have revealed that this expansion in screening age can additionally reduce lung cancer mortality by 3.2% (20,26). This expansion could improve the proportion of ethnic minorities and women eligible for screening, thus reducing the disparities caused by race and sex (27-29).
Table 2
| Association | Country | Year | Age | Smoking history | Smoking cessation |
|---|---|---|---|---|---|
| National Comprehensive Cancer Network (9) | USA | 2022 | ≥50 years | ≥20 pack-years | No time limit |
| American College of Chest Physicians (11) | USA | 2021 | 55–77 years | ≥30 pack-years | Within the past 15 years |
| 50–80 years | ≥20 pack-years | Within the past 15 years | |||
| US Preventive Services Task Force (8) | USA | 2021 | 50–80 years | ≥20 pack-years | Within the past 15 years |
| American Lung Association (10) | USA | 2018 | 50–80 years | ≥20 pack-years | Within the past 15 years |
| American Cancer Society (6) | USA | 2013 | 55–74 years | ≥30 pack-years | Within the past 15 years |
| American Association for Thoracic Surgery (7) | USA | 2012 | 55–79 years | ≥30 pack-years | No time limit |
| ≥50 years | ≥20 pack-years and added risk ≥5% of developing lung cancer within 5 yearsa | No time limit | |||
| No age limit | Patients who have been treated for a primary bronchogenic carcinoma and have completed 4 years of radiographic surveillance without evidence for recurrence | No time limit | |||
| German Radiological Society and the German Respiratory Society (25) | Germany | 2019 | 55–74 years | ≥30 pack-years | Within the past 15 years |
| ≥50 years | ≥20 pack-years and other risk factorsb | No time limit | |||
| UK National Screening Committee (23,24) | UK | 2022 | 55–74 yearsc | Having ever smoke | No time limit |
a, for instance: COPD (FEV1 <70%), environmental/occupational exposure, prior cancer/radiation therapy and genetic/family history; b, one of the following risk factors: history of lung cancer, family history of lung cancer, history of malignant ear, nose, or throat tumour or other malignant tumour associated with smoking, history of lymphoma, exposure to asbestos, chronic obstructive pulmonary disease, or pulmonary fibrosis; c, note: NHS England Targeted Lung Health Check Programme eligibility based on PLCOm2012 risk of ≥1.51% over 6 years or LLPv2 5-year risk of ≥2.5%. CT, computed tomography; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 second.
Regarding population coverage, our study found a 6.57% increase in the proportion of patients diagnosed with lung cancer when expanding the screening age from 55–80 to 50–80 years. This result was consistent with other research findings that the updated criteria could augment the proportion of the individuals eligible for lung cancer screening by 87% compared to the USPSTF criteria in 2013, which might result in an additional gain of 2,036 years of life per 100,000 people (20).
Squamous cell carcinoma was the predominant histological subtype of lung cancer between 1950 and early 1980 (30). However, recent studies have revealed an increasing trend of adenocarcinoma, which is now the main pathological subtype of lung cancer (15,16,31). This is probably attributed to the effective implementation of tobacco control policies, as studies demonstrated a close association between smoking and squamous cell carcinoma (32). In addition, alteration in the design and composition of cigarettes is thought to be a crucial factor that may increase the exposure of human peripheral airway cells to carcinogens, resulting in the development of adenocarcinoma (33,34). Our study also revealed a significant rise in the proportion of adenocarcinoma across all three age groups of patients diagnosed with lung cancer, consistent with a shift in the pathological spectrum of lung cancer. In post hoc analyses of the NLST, patients diagnosed with adenocarcinoma through low-dose CT exhibited significant survival advantages compared with those diagnosed via chest radiography; however, analogous benefits were not demonstrated in patients diagnosed with squamous cell carcinoma (12,13). Similarly, we found significant survival advantages in patients diagnosed with adenocarcinoma by expanding the initial screening age to 50 years, while no advantage was observed among patients with squamous cell carcinoma. Therefore, histological shifts should be considered when implementing lung cancer screening programs.
Sex may also be a potential factor affecting the formulation of lung cancer screening strategies (17). In subgroup analyses of the NLST and NELSON trials, greater survival benefits were observed in females than in males, indicating that relying solely on age and smoking history as inclusion criteria for screening may be inadequate (4,17,35). Similarly, another cross-sectional study also found that although the criteria recommended by USPSTF in 2021 increased female eligibility for lung cancer screening, the sex disparity might persist without “tailored eligibility criteria” (36). In our study, expanding the initial age at screening to 50 years provided significant survival advantages for male and female patients. Benefits were still found in male patients when the age criteria were extended to 45 years, while no advantage was observed among female patients, indicating that the initial age for lung cancer screening in males may be earlier compared to females. This disparity may be attributed to different levels of tobacco exposure. Although women might appear to be more likely to develop lung cancer because of cigarette exposure, study from the Centers for Disease Control and Prevention (CDC) in the United States indicate that men exhibited a higher smoking rate than women from 1965 to 2017, with rates in 2017 at 15.8% and 12.2% (37,38). A heavy smoking status of men may make them more time exposed to carcinogen and let them benefit from earlier lung cancer screening. Thus, this study supports that sex may be a potential factor affecting lung cancer screening criteria and also provides a basis for the possible need to formulate sex-based screening strategies.
This retrospective study is subject to several limitations. First, the SEER database lacks data on smoking history, which is a crucial factor in identifying individuals at high risk for lung cancer screenin, although the incidence of lung cancer is increasing among never-smokers (39). Therefore, the importance of age in screening decisions needs to be validated through subsequent multi-institutional randomized controlled trials. Second, the molecular signatures involved in lung cancer development were not investigated; therefore, we could not verify the biological disparities between males and females. Further studies are required to explore the molecular distinctiveness and heterogeneity of the sex.
Conclusions
This study demonstrated that survival advantages can be brought from lung cancer screening for patients aged 50–54, which are probably more apparent in adenocarcinoma. Younger male patients may benefit more than female patients, indicating the need for sex differences in lung cancer screening.
Acknowledgments
Funding: This study was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-475/rc
Peer Review File: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-475/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-475/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin 2023;73:17-48. [Crossref] [PubMed]
- Adams SJ, Stone E, Baldwin DR, et al. Lung cancer screening. Lancet 2023;401:390-408. [Crossref] [PubMed]
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med 2020;382:503-13. [Crossref] [PubMed]
- Haddad DN, Sandler KL, Henderson LM, et al. Disparities in Lung Cancer Screening: A Review. Ann Am Thorac Soc 2020;17:399-405. [Crossref] [PubMed]
- Wender R, Fontham ET, Barrera E Jr, et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin 2013;63:107-17. [Crossref] [PubMed]
- Jaklitsch MT, Jacobson FL, Austin JH, et al. The American Association for Thoracic Surgery guidelines for lung cancer screening using low-dose computed tomography scans for lung cancer survivors and other high-risk groups. J Thorac Cardiovasc Surg 2012;144:33-8. [Crossref] [PubMed]
- US Preventive Services Task Force. Screening for Lung Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2021;325:962-70. [Crossref] [PubMed]
- Wood DE, Kazerooni EA, Aberle D, et al. NCCN Guidelines® Insights: Lung Cancer Screening, Version 1.2022. J Natl Compr Canc Netw 2022;20:754-64. [Crossref] [PubMed]
- Thomson CC, Mckee AB. American Thoracic Society/American Lung Association Lung Cancer Screening Implementation Guide. Am J Respir Crit Care Med 2018;198:1120-1. [Crossref] [PubMed]
- Mazzone PJ, Silvestri GA, Souter LH, et al. Screening for Lung Cancer: CHEST Guideline and Expert Panel Report. Chest 2021;160:e427-94. [Crossref] [PubMed]
- Pinsky PF, Church TR, Izmirlian G, et al. The National Lung Screening Trial: results stratified by demographics, smoking history, and lung cancer histology. Cancer 2013;119:3976-83. [Crossref] [PubMed]
- Dillard TA, Patel RR, Schroeder C. Uneven Distribution of Cancer Histology in the National Lung Screening Trial. Am J Med Sci 2015;350:219-21. [Crossref] [PubMed]
- Houston KA, Mitchell KA, King J, et al. Histologic Lung Cancer Incidence Rates and Trends Vary by Race/Ethnicity and Residential County. J Thorac Oncol 2018;13:497-509. [Crossref] [PubMed]
- Flores R, Patel P, Alpert N, et al. Association of Stage Shift and Population Mortality Among Patients With Non-Small Cell Lung Cancer. JAMA Netw Open 2021;4:e2137508. [Crossref] [PubMed]
- Succony L, Rassl DM, Barker AP, et al. Adenocarcinoma spectrum lesions of the lung: Detection, pathology and treatment strategies. Cancer Treat Rev 2021;99:102237. [Crossref] [PubMed]
- Sears CR, Rivera MP. Age, Sex, Smoking, and Race: Is Progress Being Made in Lung Cancer Screening Eligibility? Chest 2021;160:31-3. [Crossref] [PubMed]
- Data from: Surveillance, Epidemiology, and End Results (SEER) Program. Available online: http://www.seer.cancer.gov
- Lewis DR, Check DP, Caporaso NE, et al. US lung cancer trends by histologic type. Cancer 2014;120:2883-92. [Crossref] [PubMed]
- Meza R, Jeon J, Toumazis I, et al. Evaluation of the Benefits and Harms of Lung Cancer Screening With Low-Dose Computed Tomography: Modeling Study for the US Preventive Services Task Force. JAMA 2021;325:988-97. [Crossref] [PubMed]
- Program SR. Expected survival life tables May7, 2020. Available online: https://seer.cancer.gov/expsurvival/
- Potter AL, Rosenstein AL, Kiang MV, et al. Association of computed tomography screening with lung cancer stage shift and survival in the United States: quasi-experimental study. BMJ 2022;376:e069008. [Crossref] [PubMed]
- NHS England. Targeted screening for lung cancer with low radiation dose computed tomography: standard protocol prepared for the targeted lung health checks programme 2019. Available online: https://www.england.nhs.uk/publication/targeted-screening-for-lung-cancer/
- UK National Screening Committee. Lung cancer. Available online: https://view-health-screening-recommendations.service.gov.uk/lung-cancer/
- Herth FJF, Reinmuth N, Wormanns D, et al. Joint Statement of the German Radiological Society and the German Respiratory Society on a Quality-Assured Early Detection Program for Lung Cancer with Low-dose CT. Pneumologie. 2019;73:573-7. [Crossref] [PubMed]
- Moyer VA. U.S. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2014;160:330-8. [Crossref] [PubMed]
- Aldrich MC, Mercaldo SF, Sandler KL, et al. Evaluation of USPSTF Lung Cancer Screening Guidelines Among African American Adult Smokers. JAMA Oncol 2019;5:1318-24. [Crossref] [PubMed]
- Wang Y, Midthun DE, Wampfler JA, et al. Trends in the proportion of patients with lung cancer meeting screening criteria. JAMA 2015;313:853-5. [Crossref] [PubMed]
- Han SS, Chow E, Ten Haaf K, et al. Disparities of National Lung Cancer Screening Guidelines in the US Population. J Natl Cancer Inst 2020;112:1136-42. [Crossref] [PubMed]
- Wynder EL, Muscat JE. The changing epidemiology of smoking and lung cancer histology. Environ Health Perspect 1995;103:143-8. [Crossref] [PubMed]
- Barta JA, Powell CA, Wisnivesky JP. Global Epidemiology of Lung Cancer. Ann Glob Health 2019;85:8. [Crossref] [PubMed]
- Li J, Li H, Zhang C, et al. Integrative analysis of genomic alteration, immune cells infiltration and prognosis of lung squamous cell carcinoma (LUSC) to identify smoking-related biomarkers. Int Immunopharmacol 2020;89:107053. [Crossref] [PubMed]
- Song MA, Benowitz NL, Berman M, et al. Cigarette Filter Ventilation and its Relationship to Increasing Rates of Lung Adenocarcinoma. J Natl Cancer Inst 2017;109:djx075. [Crossref] [PubMed]
- Thun MJ, Lally CA, Flannery JT, et al. Cigarette smoking and changes in the histopathology of lung cancer. J Natl Cancer Inst 1997;89:1580-6. [Crossref] [PubMed]
- Lung Cancer Incidence and Mortality with Extended Follow-up in the National Lung Screening Trial. J Thorac Oncol 2019;14:1732-42. [Crossref] [PubMed]
- Reese TJ, Schlechter CR, Potter LN, et al. Evaluation of Revised US Preventive Services Task Force Lung Cancer Screening Guideline Among Women and Racial/Ethnic Minority Populations. JAMA Netw Open 2021;4:e2033769. [Crossref] [PubMed]
- MacRosty CR, Rivera MP. Lung Cancer in Women: A Modern Epidemic. Clin Chest Med 2020;41:53-65. [Crossref] [PubMed]
- United States Public Health Service Office of the Surgeon General, National Center for Chronic Disease Prevention, Health Promotion Office on Smoking, et al. Publications and Reports of the Surgeon General. Smoking Cessation: A Report of the Surgeon General. Washington (DC): US Department of Health and Human Services; 2020.
- DeRouen MC, Canchola AJ, Thompson CA, et al. Incidence of Lung Cancer Among Never-Smoking Asian American, Native Hawaiian, and Pacific Islander Females. J Natl Cancer Inst 2022;114:78-86. [Crossref] [PubMed]


