
Influence of pleural invasion on survival in pathologic T3–4N0M0 non-small cell lung cancer: a propensity score matching study based on the Surveillance, Epidemiology, and End Results database
Highlight box
Key findings
• Pleural invasion (PI) is a risk factor for poor prognosis in pT3–4N0M0 non-small cell lung cancer (NSCLC).
• No significant survival differences were observed between patients with T3 diseases and PI and those with T4 disease without PI.
What is known and what is new?
• Visceral pleural invasion (VPI) is an additional histologic descriptor in the staging system for T2 categories. Some studies suggest that pT3N0M0 with chest wall infiltration (CWI) could be upstaged to pT4; however, the prognostic impact of PI, encompassing VPI, parietal pleura invasion, and CWI, in patients with T3–4 NSCLC remains uncertain.
• Our findings study that PI has potential as an additional histologic descriptor in the new staging system for the T3–4 categories.
What is the implication, and what should change now?
• Pathologic T3N0M0 tumors with PI could be upstaged to the T4 category (stage IIIA) in the future edition of the tumor, node, metastasis classification.
Introduction
Lung cancer represents the most frequently diagnosed and leading cause of cancer-related death worldwide (1). Approximately 80–85% of patients with lung cancer are diagnosed with non-small cell lung cancer (NSCLC) (2). Surgical resection, whenever possible, is generally the preferred treatment modality for early-stage NSCLC (3). The 5-year survival rate for patients with NSCLC ranges from 9% to 65%, with this variability being attributable to stage and geographic differences (4).
Pleural invasion (PI) is known to be one of the most important prognostic factors in patients undergoing complete lung cancer resection (5). In 1997, it was incorporated as a negative prognosticator within the fifth edition of tumor, node, metastasis (TNM) classification criteria (6). The International Association for the Study of Lung Cancer (IASLC) recommends classifying PI status as follows: PL0, no evidence of visceral pleural invasion (VPI) surpassing the elastic layer; PL1, invasion surpassing the elastic layer; PL2, invasion to the pleural surface; and PL3, invasion to the parietal pleural, thoracic wall, or both (7). PL1 and PL2 both represent invasion of the VPI, while PL3 represents parietal pleural invasion (PPI). The seventh and eighth editions of the TNM staging system introduced VPI as a size-independent T2 factor, upstaging tumours ≤3 cm to T2a. PPI is a T3 descriptor, as no prognostic differences have been found regarding tumors macroscopically invading the chest wall (8-10).
However, recent IASLC studies have shown that pathologic chest wall or parietal pleura involvement results in poorer survival than other T3 descriptors, with survival rates comparable to those of T4 (11). This topic remains controversial, and it is still unclear whether VPI impacts overall survival (OS), equivalent to PPI in the T3 category. This study thus aimed to determine the prognostic influence of PI and the possibility of modifying the TNM classification of NSCLC. Using the Surveillance, Epidemiology, and End Results (SEER) database, we compared the oncologic outcomes according to PI status in patients who had undergone resection for pT3–4N0M0 NSCLC. We present this article in accordance with the STROBE reporting checklist (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-860/rc).
Methods
Data collection
We conducted a survival analysis of the patients in SEER database with custom data and additional treatment fields. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and included patients with an NSCLC diagnosis who had undergone radical surgery between 2010 and 2019. The flowchart of patient selection is shown in Figure S1. Exclusion criteria were distant metastasis at diagnosis, lack of available survival information, TNM classification, age, tumor size, stage, chemotherapy or radiotherapy status, node involvement, PI, and histologically confirmed resection. Based on the information in the SEER database, patients with NSCLC were reclassified according to the eighth edition of the TNM classification, and those which did not match the TNM staging were excluded (12). The PI status was obtained from the collaborative stage site-specific factor 2 variables and collaborative stage extension.
Variable definition
In this observational population, we extracted the following information: population baseline data (race, age, sex, cause of death, survival), tumor characteristics (tumor location, histological subtypes, T category, PI) and treatment (resection, radiotherapy, and chemotherapy). In addition, the different histologic types were collected into three categories including squamous cell carcinoma, adenocarcinoma, and other [e.g., neuroendocrine cancers (NEC), neuroendocrine tumor (NET), spindle cell carcinoma]. Surgical resection was divided into wedge resection, segmental resection, lobectomy, and pneumonectomy. According to different T categories and PI status, tumors were divided into six groups (T3PL0, T3PL1/2, T3PL3, T4PL0, T4PL1/2, T4PL3) or four groups (T3 without PI, T3 PI, T4 without PI, T4 PI).
Statistical analysis
Categorical variables were expressed frequencies and percentages, while continuous variables were expressed as the mean and standard deviation or as the median and interquartile range. OS was assessed using the Kaplan-Meier method and compared using the log-rank test; OS was defined as the time interval between surgery and death. The Cox proportional hazard ratios model assessed the variables that significantly influenced OS in multivariable analysis. Variables with two-sided P values ≤0.05 were considered statistically significant. All variables with a P value <0.10 or otherwise considered clinically relevant were included in a multivariable model in stepwise fashion.
Propensity score matching (PSM) was used to balance the potential bias between groups. The baseline characteristics of patients included age, race, sex, histological type, tumor location, surgical type, chemotherapy, and radiotherapy. This study used the nearest-neighbors method to compare the groups (matching ratio =1:1, caliper =0.02) based on the propensity scores. Statistical analysis was performed with the R version 3.6.2 (The R Foundation for Statistical Computing).
Results
Characteristics of patients
A total of 9,185 surgically treated patients with NSCLC met the inclusion criteria. The median follow-up time after surgery was 33 months (interquartile range: 14–63 months). From the total number of patients, 1,770 (19.27%) had VPI and 1,007 (10.96%) had PPI (Table 1). The proportions of patient’s gender, age, race, histologic type, T category, tumor location, chemotherapy, and radiotherapy between patients without and with PI were significantly different (P<0.001). The differences in the proportion of surgical types between patients with tumors without and with PI were not significantly different (P=0.68). Compared with that of squamous cell carcinoma, the proportion of pleural involvement in adenocarcinoma was lower (29.01 vs. 36.18), with a higher proportion of VPI (20.26 vs. 19.71) and a lower proportion of PPI (8.75 vs. 16.46). With worse PI, the proportions of patients undergoing radiotherapy and chemotherapy significantly increased.
Table 1
| Variable | PL0 (N=6,408) | PL1/2 (N=1,770) | PL3 (N=1,007) | SMD | P value |
|---|---|---|---|---|---|
| Gender | 0.13 | <0.001* | |||
| Female | 3,342 (52.2) | 867 (49.0) | 430 (42.7) | ||
| Male | 3,066 (47.8) | 903 (51.0) | 577 (57.3) | ||
| Age, years | 68.14±9.80 | 69.59±9.36 | 67.97±9.23 | 0.11 | <0.001* |
| Race | 0.11 | <0.001* | |||
| White | 5,417 (84.5) | 1,438 (81.2) | 876 (87.0) | ||
| Black | 543 (8.5) | 167 (9.4) | 69 (6.9) | ||
| Other | 448 (7.0) | 165 (9.3) | 62 (6.2) | ||
| Histologic type | 0.28 | <0.001* | |||
| Adenocarcinoma | 3,912 (61.0) | 1,117 (63.1) | 482 (47.9) | ||
| Squamous cell carcinoma | 1,686 (26.3) | 521 (29.4) | 435 (43.2) | ||
| Other | 810 (12.6) | 132 (7.5) | 90 (8.9) | ||
| T category | 0.21 | <0.001* | |||
| T3 | 4,371 (68.2) | 1,140 (64.4) | 787 (78.2) | ||
| T4 | 2,037 (31.8) | 630 (35.6) | 220 (21.8) | ||
| Tumor size | 0.48 | <0.001* | |||
| ≤3 cm | 2,491 (38.9) | 486 (27.5) | 288 (28.6) | ||
| >3 cm and ≤5 cm | 627 (9.8) | 270 (15.3) | 352 (35.0) | ||
| >5 cm and ≤7 cm | 2,159 (33.7) | 626 (35.4) | 206 (20.5) | ||
| >7 cm | 1,131 (17.6) | 388 (21.9) | 161 (16.0) | ||
| Tumor location | 0.39 | <0.001* | |||
| Right upper lobe | 1,838 (28.7) | 561 (31.7) | 426 (42.3) | ||
| Right middle lobe | 325 (5.1) | 80 (4.5) | 23 (2.3) | ||
| Right lower lobe | 1,347 (21.0) | 342 (19.3) | 77 (7.6) | ||
| Left upper lobe | 1,400 (21.8) | 410 (23.2) | 345 (34.3) | ||
| Left lower lobe | 1,046 (16.3) | 245 (13.8) | 103 (10.2) | ||
| Other | 452 (7.1) | 132 (7.5) | 33 (3.3) | ||
| Surgical type | 0.05 | 0.68 | |||
| Wedge resection | 797 (12.4) | 208 (11.8) | 135 (13.4) | ||
| Segmentectomy | 192 (3.0) | 51 (2.9) | 30 (3.0) | ||
| Lobectomy | 5,331 (83.2) | 1,487 (84.0) | 834 (82.8) | ||
| Pneumonectomy | 88 (1.4) | 24 (1.4) | 8 (0.8) | ||
| Chemotherapy | 0.21 | <0.001* | |||
| Yes | 2,268 (35.4) | 767 (43.3) | 513 (50.9) | ||
| No | 4,140 (64.6) | 1,003 (56.7) | 494 (49.1) | ||
| Radiotherapy | 0.45 | <0.001* | |||
| Yes | 506 (7.9) | 236 (13.3) | 342 (34.0) | ||
| No | 5,902 (92.1) | 1,534 (86.7) | 665 (66.0) |
Data are presented as n (%) or mean ± standard deviation. *, significant at P<0.001. PL, pleural layer; SMD, standardized mean difference.
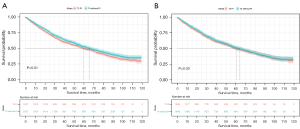
OS in groups with different T categories and PI statuses
Tumors were stratified into six groups according to different T categories and PI statuses. In patients with T4 tumors, the 5-year OS rates of T4 PL0, PL1/2, and PL3 were 52.8%, 38.4%, and 31.7%, respectively. Figure 1A indicates that patients’ OS significantly decreased with worsening PI (P<0.001). As shown in Table S1, both univariable and multivariable survival analyses for patients with T4 tumors indicated that the presence of pleural involvement was significantly associated with worse prognosis [PL1/2 vs. PL0: hazard ratio (HR) =1.42, 95% confidence interval (CI): 1.25–1.62, P<0.001; PL3 vs. PL0: HR =1.91, 95% CI: 1.58–2.30, P<0.001]. Furthermore, age, gender, chemotherapy, and radiotherapy were identified as significant predictors of OS.
In patients with T3 tumors, the 5-year OS rates of T3PL0, PL1/2, and PL3 subgroups were 60.9%, 52.2%, and 46.5%, respectively. Figure 1B indicates that patients’ OS significantly decreased with worsening PI (P<0.001). As shown in Table S2, both univariable and multivariable survival analyses for patients with T3 tumors indicated that the presence of pleural involvement was significantly associated with worse prognosis (PL1/2 vs. PL0: HR =1.26, 95% CI: 1.13–1.41, P<0.001; PL3 vs. PL0: HR =1.34, 95% CI: 1.19–1.51, P<0.001). Besides age, gender, chemotherapy, and radiotherapy, histologic and surgical types were also identified as significant predictors of OS.

OS after PSM in patients with stage T3 and T4 disease
The PSM model included eight variables: age, gender, race, histologic type, tumor location, surgical type, chemotherapy, and radiotherapy. After PSM, the discrepancy of all variables was balanced (see Tables S3-S6).
OS after PSM for the T4PL0, T4PL1/2, and T4PL3 subgroups
After PSM, 626 matched pairs were divided into the T4PL0 and T4PL1/2 subgroups, and 196 matched pairs were divided into the T4PL1/2 and T4PL3 subgroups. A significant difference in OS was found between the T4PL0 and T4PL1/2 groups (P<0.001; Figure 2A). However, there was no significant difference in OS between the T4PL1/2 and T4PL3 subgroups (P=0.25; Figure 2B).

OS after PSM for the T3PL0, T3PL1/2, and T3PL3 subgroups
After PSM, 1,138 matched pairs were classified into the T3PL0 and T3PL1/2 subgroups, and 663 matched pairs were classified into the T3PL1/2 and T3PL3 subgroups. Analysis of OS revealed a statistically significant difference between the T3PL0 and T3PL1/2 groups (P=0.001; Figure 2C). However, the OS comparison between the T3PL1/2 and T3PL3 groups did not show a statistically significant difference (P=0.12; Figure 2D).
OS in patients with T3 but not PI, T3 with PI, T4 but not PI, and T4 with PI
No significant differences were found between the T4PL1/2 and T4PL3 subgroups or between the T3PL1/2 and T3PL3 subgroups. Consequently, these groups were merged to form two aggregated cohorts: T4 PI and T3 PI.
Subsequent stratification yielded four distinct cohorts: T3 without PI, T3 with PI, T4 without PI, and T4 with PI; the 5-year OS rates observed for these groups were 60.9%, 49.6%, 52.8%, and 36.6% (P<0.001), respectively. Notably, T3 with PI exhibited a lower OS than did T4 without PI (Figure 3).

OS after PSM in the T3 PI and T4 without PI subgroups
PSM was conducted to elucidate the differences between the T3 PI and T4 without PI subgroups. After PSM, 1,646 matched pairs were divided into the T3 PI and T4 without PI subgroups (Table S7). Before PSM, a significant difference in OS was observed between the T3 PI and T4 without PI and subgroups (P=0.01; Figure 4A). However, after PSM, no significant differences in OS were revealed between the two matched groups (P=0.30; Figure 4B).
Discussion
During the past several decades, several studies have demonstrated that patients with VPI have worse outcomes, with a higher rate of mediastinal lymph node metastases, malignant pleural effusion, and postoperative recurrence (13-16). Despite concerns regarding the effects of VPI severity on T category, the eighth edition of TNM classification states that only tumors ≤3 cm (T1) with VPI should be upgraded to T2a, whereas VIP is not a descriptor for tumors >3 cm (10). However, Yoshida et al. noted the substantial impact of VPI and suggested that tumors smaller than 7 cm be reclassified to a higher T stage in the forthcoming TNM staging system revision (17). Yang et al. reported that the OS of patients with VPI and N0 tumors is associated with a poorer OS than that of patients with N1 or N2 tumors (18). Several studies suggest that patients with VPI and tumors larger than 3 cm should potentially be upgraded (7,19-22). PPI is a T3 descriptor that is similar to chest wall infiltration (CWI), as no prognostic differences have been found for tumors macroscopically invading the chest wall (23). Furthermore, the classification of T3 tumors with PL3 or CWI did not escalate with the increased extent of PI (10). A recent study suggests an upward revision of its category (24).
In this series, we analyzed the impact of PI on the survival of patients with NSCLC using a large dataset from the SEER database. Considering the differences between the T3N0M0 and T4N0M0 tumors (in stages IIB and IIIA, respectively), we proposed a method to incorporate PI into the T status in the revised TNM classification. We performed multivariable analysis to exclude the effects of other factors and found that the independent prognostic factors of T4N0M0 were pleural involvement status, age, gender, chemotherapy, and radiotherapy; meanwhile, the independent prognostic factors of T3N0M0 were pleural involvement status, age, gender, chemotherapy and radiotherapy, histologic type, and surgical type.
Based on the multivariable analysis results, we applied propensity score PSM to address variable imbalances between the subgroups, thus more accurately characterizing the survival differences of PI across these groups. The analysis indicated that all levels of PI (VPI, PPI) correlated with poorer prognoses. However, no survival difference was observed between the VPI and PPI groups in T3–4N0M0 (Figure 2B,2D).
Therefore, we divided the participants into four groups based on the presence or absence of PI. After PSM and survival analysis, we found that patients with PI had worse survival across all stages. Notably, the 5-year OS for patients with T3 PI tumors was 50.0% compared to 51.8% for T4 without PI, and no significant difference in survival was found (before PSM: P=0.01; after PSM: P=0.30), which suggested that T3 tumors with PI should be upstaged to T4.
Additionally, VPI was observed in 18.1% of T3N0M0 tumors, significantly less frequently than in T4N0M0 tumors (21.8%), which is consistent with previously reported rates which range from 11.5% to 26.8% (14,25-27). Other studies have indicated that VPI increases with tumor size (19,26,28), significantly so in tumor sizes larger than 3 cm (29). Multiple factors affect survival outcomes: as the influence of one factor (tumor size) increases, another factor (PI) may correspondingly decrease. This may explain why statistical analysis revealed no significant survival differences between the VPI and PPI groups.
The extent of VPI can be described as PL1 and PL2, but it remains unclear whether the distinction between PL1 and PL2 is relevant to survival. Kawase et al. and Adachi et al. found no evidence of a significant survival difference between PL1 and PL2 regardless of the status of lymph node involvement (22,30). However, other studies have reported a significant difference in OS between patients with PL1 and PL2 (23,31,32). We did not perform stratification of OS with PL1 and PL2 combined with tumor size, which was a limitation of our study. Therefore, a prognostic model that includes the detailed depth of VPI should be constructed in subsequent research.
Moreover, the chest wall comprises the parietal pleura, soft tissue, intercostal muscles, and ribs (33). The SEER database does not clearly differentiate between PL3 and CWI. Considering the presence of PPI in patients with CWI, Matsuoka et al. found no significant difference in survival rates across the different extents of CWI (parietal pleura: 32.5%; subpleural tissue: 30.0%; ribs: 38.5%) (8). Additionally, in recent research by Ugalde et al., no significant differences in OS associated with PL3 and CWI as T3 descriptors (log-rank P=0.26) was found (24). In the IASLC’s recommendations for the ninth edition TNM classification, clinical T3-PPI/CWI aligns well with the other cT3 descriptors; however, pathologic T3-PPI/CWI corresponds to pT4. Due to the inconsistent findings, they did not recommend reclassifying T3-PPI/CWI (11). In our study, the PL3 and CWI subgroups were consolidated, with the results being consistent with the related IASLC studies. Additionally, we found no difference in long-term survival between pathologic T3PL1/2 and T3PL3, T3 PI comparable to T4 (Figures 2D,4B).
This study had certain limitations which should be noted. First, as a retrospective study spanning over a decade, selection bias could not be ruled out. Second, SEER does not include detailed information on the patients’ condition, smoking history, postoperative complications, gene mutation detection, programmed cell death ligand 1 (PD-L1) detection, adjuvant therapeutic agents and dose, which are necessary for prognosis. Additionally, SEER does not specify residual tumor classification (R0, R1, or R2), which is crucial in understanding the oncological outcomes of different surgical approaches, particularly in comparing wedge resection, segmentectomy, and lobectomy. Finally, due to insufficient data on cancer recurrence and disease-free survival, we were unable to assess the relationship between progression-free survival and PI. Fortunately, the clinical information is standard. Reasonable and scientific PSM analysis methods were applied in our study to reduce the covariate imbalance and selection bias, and the conclusions drawn from the findings are sound.
Conclusions
PI was found to be a risk factor for poor prognosis in patients with pT3–4N0M0 NSCLC. Our results recommend future studies exploring the prognostic value of various T3–4 subcategories to allow PI to be separated from other T descriptors and confounders.
Acknowledgments
The preliminary results of this study were presented in part at the 31st European Conference on General Thoracic Surgery of the European Society of Thoracic Surgeons, Milan, Italy on June 4–6, 2023 (Oral presentation, O-079).
The authors would like to thank Ramón Rami-Porta, a thoracic surgeon from Hospital Universitari Mútua Terrassa, Terrasa, Spain, for reviewing the manuscript and providing relevant comments on different issues of the TNM classification of lung cancer.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-860/rc
Peer Review File: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-860/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-860/coif). W.Z. receives financial support from China Scholarship Council during his studies in Germany. H.B. is from Charité Research Organisation GmbH (CRO), Berlin, Germany. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2024;74:229-63. [Crossref] [PubMed]
- Lung Cancer Statistics | How Common is Lung Cancer? Accessed April 20, 2024. Available online: https://www.cancer.org/cancer/types/lung-cancer/about/key-statistics.html
- Vansteenkiste J, Crinò L, Dooms C, et al. 2nd ESMO Consensus Conference on Lung Cancer: early-stage non-small-cell lung cancer consensus on diagnosis, treatment and follow-up. Ann Oncol 2014;25:1462-74. [Crossref] [PubMed]
- Lung Cancer Survival Rates | 5-Year Survival Rates for Lung Cancer. Accessed April 20, 2024. Available online: https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/survival-rates.html
- Brewer LA, Bai AF, Little JN, et al. Carcinoma of the lung; practical classification for early diagnosis and surgical treatment. J Am Med Assoc 1958;166:1149-55. [Crossref] [PubMed]
- Mountain CF. Revisions in the International System for Staging Lung Cancer. Chest 1997;111:1710-7. [Crossref] [PubMed]
- Travis WD, Brambilla E, Rami-Porta R, et al. Visceral pleural invasion: pathologic criteria and use of elastic stains: proposal for the 7th edition of the TNM classification for lung cancer. J Thorac Oncol 2008;3:1384-90.
- Matsuoka H, Nishio W, Okada M, et al. Resection of chest wall invasion in patients with non-small cell lung cancer. Eur J Cardiothorac Surg 2004;26:1200-4. [Crossref] [PubMed]
- Goldstraw P, Crowley J, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2007;2:706-14. [Crossref] [PubMed]
- Goldstraw P, Chansky K, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2016;11:39-51. [Crossref] [PubMed]
- Van Schil PE, Asamura H, Nishimura KK, et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: Proposals for the Revisions of the T-Descriptors in the Forthcoming Ninth Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2024;19:749-65.
- Brierley JD, Gospodarowicz MK, Wittekind Ch. editers. UICC TNM Classification of Malignant Tumors, 8th ed. Oxford: Wiley Blackwell; 2017:105-112.
- Ohtaki Y, Hishida T, Yoshida J, et al. The clinical outcome of non-small cell lung cancer patients with adjacent lobe invasion: the optimal classification according to the status of the interlobar pleura at the invasion point. Eur J Cardiothorac Surg 2013;43:302-9. [Crossref] [PubMed]
- Shimizu K, Yoshida J, Nagai K, et al. Visceral pleural invasion is an invasive and aggressive indicator of non-small cell lung cancer. J Thorac Cardiovasc Surg 2005;130:160-5. [Crossref] [PubMed]
- Zhang H, Lu C, Lu Y, et al. The predictive and prognostic values of factors associated with visceral pleural involvement in resected lung adenocarcinomas. Onco Targets Ther 2016;9:2337-48. [Crossref] [PubMed]
- Tian D, Pei Y, Zheng Q, et al. Effect of visceral pleural invasion on the prognosis of patients with lymph node negative non-small cell lung cancer. Thorac Cancer 2017;8:97-105. [Crossref] [PubMed]
- Yoshida J, Nagai K, Asamura H, et al. Visceral pleura invasion impact on non-small cell lung cancer patient survival: its implications for the forthcoming TNM staging based on a large-scale nation-wide database. J Thorac Oncol 2009;4:959-63. [Crossref] [PubMed]
- Yang H, Mei T. Prognostic significance of visceral pleural invasion in patients with surgically resected small-cell lung cancer: a population-based study. Jpn J Clin Oncol 2022;52:1045-55. [Crossref] [PubMed]
- David E, Thall PF, Kalhor N, et al. Visceral pleural invasion is not predictive of survival in patients with lung cancer and smaller tumor size. Ann Thorac Surg 2013;95:1872-7; discussion 1877. [Crossref] [PubMed]
- Jiang L, Liang W, Shen J, et al. The impact of visceral pleural invasion in node-negative non-small cell lung cancer: a systematic review and meta-analysis. Chest 2015;148:903-11. [Crossref] [PubMed]
- Kang JH, Kim KD, Chung KY. Prognostic value of visceral pleura invasion in non-small cell lung cancer. Eur J Cardiothorac Surg 2003;23:865-9. [Crossref] [PubMed]
- Kawase A, Yoshida J, Ishii G, et al. Visceral pleural invasion classification in non-small cell lung cancer. J Thorac Oncol 2010;5:1784-8. [Crossref] [PubMed]
- Rami-Porta R, Bolejack V, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for the Revisions of the T Descriptors in the Forthcoming Eighth Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2015;10:990-1003.
- Ugalde Figueroa PA, Marques E, Cilento VJ, et al. Completeness of Resection and Long-Term Survival of Patients Undergoing Resection for Pathologic T3 NSCLC: An International Association for the Study of Lung Cancer Analysis. J Thorac Oncol 2024;19:141-52. [Crossref] [PubMed]
- Hung JJ, Wang CY, Huang MH, et al. Prognostic factors in resected stage I non-small cell lung cancer with a diameter of 3 cm or less: visceral pleural invasion did not influence overall and disease-free survival. J Thorac Cardiovasc Surg 2007;134:638-43. [Crossref] [PubMed]
- Manac'h D, Riquet M, Medioni J, et al. Visceral pleura invasion by non-small cell lung cancer: an underrated bad prognostic factor. Ann Thorac Surg 2001;71:1088-93. [Crossref] [PubMed]
- Takizawa T, Terashima M, Koike T, et al. Lymph node metastasis in small peripheral adenocarcinoma of the lung. J Thorac Cardiovasc Surg 1998;116:276-80. [Crossref] [PubMed]
- Yanagawa N, Shiono S, Abiko M, et al. Prognostic impact and initial recurrence site of lymphovascular and visceral pleural invasion in surgically resected stage I non-small-cell lung carcinoma. Eur J Cardiothorac Surg 2013;44:e200-6. [Crossref] [PubMed]
- Yilmaz A, Duyar SS, Cakir E, et al. Clinical impact of visceral pleural, lymphovascular and perineural invasion in completely resected non-small cell lung cancer. Eur J Cardiothorac Surg 2011;40:664-70. [Crossref] [PubMed]
- Adachi H, Tsuboi M, Nishii T, et al. Influence of visceral pleural invasion on survival in completely resected non-small-cell lung cancer. Eur J Cardiothorac Surg 2015;48:691-7; discussion 697. [Crossref] [PubMed]
- Kudo Y, Saji H, Shimada Y, et al. Impact of visceral pleural invasion on the survival of patients with non-small cell lung cancer. Lung Cancer 2012;78:153-60. [Crossref] [PubMed]
- Hung JJ, Jeng WJ, Hsu WH, et al. Prognostic significance of the extent of visceral pleural invasion in completely resected node-negative non-small cell lung cancer. Chest 2012;142:141-50. [Crossref] [PubMed]
- Facciolo F, Cardillo G, Lopergolo M, et al. Chest wall invasion in non-small cell lung carcinoma: a rationale for en bloc resection. J Thorac Cardiovasc Surg 2001;121:649-56. [Crossref] [PubMed]


