
Prognostic value of ground-glass opacity on computed tomography for patients with pathological stage IA3 lung adenocarcinoma: a multicenter retrospective cohort study
Highlight box
Key findings
• Presence of ground-glass opacity (GGO) was an effective prognostic factor for patients with micropapillary (MIP)-negative pathological stage IA3 lung adenocarcinoma (LUAD) for up to 2 years.
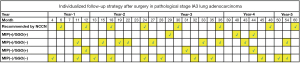
• For patients with pathological stage IA3 LUAD, we recommend the following number of follow-up sessions within 5 years based on their MIP and GGO status: MIP(+)-GGO(+): 3 follow-up sessions; MIP(+)-GGO(−): 9 follow-up sessions; MIP(−)-GGO(+): 3 follow-up sessions; MIP(−)-GGO(−): 11 follow-up sessions.
What is known and what is new?
• GGO is generally associated with better prognosis in patients with early-stage LUAD, whereas MIP is linked to a higher recurrence risk and worse outcomes.
• This study was the first to identify the positive prognostic value of GGO in patients with MIP-negative IA3 LUAD and to introduce a personalized follow-up strategy based on recurrence risk.
What is the implication, and what should change now?
• The findings suggest that follow-up strategies for patients with IA3 LUAD should consider both GGO and MIP status to more effectively manage recurrence risks. Future clinical practice should implement stratified follow-up plans tailored to GGO and MIP profiles to improve prognosis and patient outcomes.
Introduction
Surgical resection is a potentially curative option for early-stage lung adenocarcinoma (LUAD) (1,2). However, most patients are imperiled by recurrence and cancer-related mortality. Computed tomography (CT) imaging can reveal the different patterns of LUAD, encompassing pure solid nodules, pure ground-glass opacities (GGOs), and part-solid nodules (3,4). Pathologically, these tumors exhibit lepidic growth patterns in addition to acinar, papillary, solid, and micropapillary (MIP) subtypes (5).
According to consensus guidelines of the International Lung Cancer Research Association, the American Thoracic Association, and the European Respiratory Association, tumors characterized by an MIP component are at a high risk of recurrence (6-8). Even the minor presence of such component is linked to lymph node metastases, increased invasiveness, pleural invasion, and early disease relapse, significantly affecting patients’ prognosis, The presence of the MIP component in LUAD is linked to increased invasiveness, high proliferative activity, and a distinct molecular profile that often results in poor prognosis (9-11). Presence of GGO has been reported to be an independent prognostic factor for early LUAD. GGO features, including atypical adenomatous hyperplasia (AAH), minimally invasive adenocarcinoma (MIA), and lepidic growth patterns, are often associated with less aggressive tumor behavior, slower growth, and lower metastatic potential. These characteristics contribute to a more favorable prognosis, particularly in early-stage tumors (12-14). However, prior single-center studies have indicated that the GGO component can independently reflect a favorable prognosis in patients with pathological stage IA1/IA2 LUAD but does not significantly impact the prognosis of patients with pathological stage IA3 LUAD (15,16).
Hence, the relevance of the GGO component to the prognosis of pathological stage IA3 LUAD and the impact of MIP status on the prognostic value of GGO remain areas of uncertainty. Furthermore, current guidelines recommend uniform follow-up strategies for all patients with pathological stage IA3 LUAD despite varying recurrence risks and recurrence timelines (17). Therefore, we sought to understand whether and to what extent the MIP component of the MIP component influences the prognostic significance of GGO in predicting outcomes for patients with pathological stage IA3 LUAD in order to better inform the tailoring of monitoring programs. We present this article in accordance with the STROBE reporting checklist (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-923/rc).
Methods
Patients
In this multicenter retrospective study, we screened data from 466 patients with pathological IA3 stage LUAD admitted to four institutions in China (Fujian Medical University Union Hospital, The First Hospital of Putian, Nanping First Hospital Affiliated to Fujian Medical University, Ningde Municipal Hospital of Ningde Normal University) between July 2012 and July 2020. The sample size was determined by the number of eligible cases from these institutions during the study period. To ensure a representative cohort, all patients were consecutively enrolled based on predefined inclusion and exclusion criteria. The inclusion criteria were: (I) patients who underwent radical surgery and (II) those who underwent lobectomy. The exclusion criteria were: (I) multiple primary LUADs; (II) wedge or segmental resection; (III) a lack of clinicopathological information or follow-up data; (IV) mortality within 1 month postoperatively; and (V) non-tumor-related death. After applying these criteria, a total of 411 patients were included in the study. A flowchart of patient enrollment in this study is shown in Figure S1.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of the Fujian Medical University Union Hospital (IRB No. 2023KY190). All participating hospitals were informed and agreed with this study. The requirement for patients’ informed consent was waived as it was a retrospective research. Data on clinicopathological variables were obtained by reviewing patient medical records. Gender, age at diagnosis, smoking history, tumor size, MIP component, and epidermal growth factor receptor (EGFR) mutation were collected.
Radiologic evaluation
All patients included in the study received CT scan were conducted using 64-detector-row CT scanners (SOMATOM Sensation, Siemens Healthineers, Erlangen, Germany) within 30 days prior to surgery. The chest CT scans were evaluated in the lung window (a window width of 1,400 Hounsfield units) by two independent investigators. Areas with a hazy, high-density appearance, with the outlines of the bronchi and blood vessels being conserved, were classified as having a GGO component. Conversely, a lung mass completely enveloping the bronchi and vessels was considered to be a solid component. Depending on the presence of a GGO component, patients were categorized into a GGO group and a non-GGO group (18). If discrepancies arose between the original diagnostic reports and the interpretations by the two investigators, they were resolved through discussion.
Histopathologic evaluation
The pathological diagnosis of LUAD in this study adhered to the 2015 criteria set by the World Health Organization (WHO) for lung cancer. MIP was pathologically defined by the presence of small, nipple-like epithelial structures without a fibrous vascular core. A positive MIP status was assigned when the MIP component constituted more than 5% of the total tumor tissue, whereas a negative MIP status corresponded to cases where the component constituted less than 5%. To ensure consistency and reliability in the evaluation of the MIP component, multiple experienced pathologists participated in the pathological assessment of the tumor samples. Specifically, three pathologists, all with extensive experience in lung cancer pathology, independently assessed the presence and proportion of the MIP component. To minimize inter-observer variability, a consensus meeting was held in which discrepancies between the pathologists’ evaluations were discussed and resolved. This process was employed to ensure that the assessment of the MIP component was as accurate and standardized as possible.
Follow-up
According to the posttreatment recommendations provided by the National Comprehensive Cancer Network (NCCN) guidelines, patients with pathological stage IA3 LUAD were monitored through outpatient visits or telephone consultations (17). Tumor metastasis or recurrence was confirmed postoperatively on the basis of radiological findings or histopathological examination. Recurrence-free survival (RFS) is the duration from surgery until the occurrence of tumor relapse or distant metastasis, while cancer-specific survival (CSS) is the time span from surgery until death resulting directly from the tumor. The final follow-up was extended until July 2021 or the patient’s death.
Statistical analysis
To compare the characteristics between the GGO group and the non-GGO and between the MIP-positive group and MIP-negative group, the t-test and chi-square tests were used for continuous and categorical variables, respectively. Log-rank tests and Kaplan-Meier were employed to evaluate survival differences between different groups. Factors significantly associated with RFS and CSS (All P values tested were bilateral, with a difference of P<0.05 being statistically significant.) were identified through Cox univariate regression analysis included in the multivariate analysis during follow-up.
Time-dependent multivariate analysis assessed the prognostic significance of these factors in relation to RFS and CSS. The life-table method was used to examine recurrence dynamics, specifically calculating the probability of recurrence within 1-month intervals. Recurrence rates were expressed as the risk per patient per month.
All the tests were two-tailed with statistical significance set at P<0.05, and all assessments were conducted using SPSS 26 (IBM Corp., Armonk, NY, USA) and R 3.6.1 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
A total of 411 eligible patients were enrolled, 51.3% (211/411) of whom were males and 48.7% (200/411) females. The average tumor size was 2.46±0.26 cm. Approximately 50.6% (208/411) of patients were in the GGO group and 49.4% (203/411) were in the non-GGO group. The two groups differed significantly in terms of preoperative carcinoembryonic antigen levels (P=0.045), tumor size (P=0.004), and MIP status (P=0.01). However, they did not differ significantly in terms of body mass index (P=0.86), sex (P=0.46), age (P=0.75), preoperative symptoms (P=0.11), family history (P=0.16), EGFR mutation (P=0.31), or lymph node dissection (P=0.10) (Table 1).
Table 1
| Characteristics | Total (n=411) | GGO component | P value | |
|---|---|---|---|---|
| Absence (n=208) | Presence (n=203) | |||
| Sex | 0.46 | |||
| Female | 200 (48.7) | 105 (50.5) | 95 (46.8) | |
| Male | 211 (51.3) | 103 (49.5) | 108 (53.2) | |
| Age (years) | 0.75 | |||
| <65 | 258 (62.8) | 129 (62.0) | 129 (63.5) | |
| ≥65 | 153 (37.2) | 79 (38.0) | 74 (36.5) | |
| BMI (kg/m2) | 23.5±2.89 | 23.54±2.84 | 23.60±2.94 | 0.86 |
| Smoke history | 0.87 | |||
| No | 292 (71.0) | 147 (70.7) | 145 (71.4) | |
| Yes | 119 (29.0) | 61 (29.3) | 58 (28.6) | |
| Family history | 0.16 | |||
| No | 393 (95.6) | 196 (94.2) | 197 (97.0) | |
| Yes | 18 (4.4) | 12 (5.8) | 6 (3.0) | |
| Preoperative CEA (ng/mL) | 0.045 | |||
| <5 | 270 (65.7) | 127 (61.1) | 143 (70.4) | |
| ≥5 | 141 (34.3) | 81 (38.9) | 60 (29.6) | |
| Preoperative symptoms | 0.11 | |||
| No | 293 (71.3) | 141 (67.8) | 152 (74.9) | |
| Yes | 118 (28.7) | 67 (32.2) | 51 (25.1) | |
| Tumor size (cm) | 2.46±0.26 | 2.50±0.26 | 2.42±0.25 | 0.004 |
| Lymph node dissection | 16.57±8.00 | 17.22±8.24 | 15.91±7.72 | 0.10 |
| MIP component | 0.01 | |||
| <5% | 319 (77.6) | 151 (72.6) | 168 (82.8) | |
| ≥5% | 92 (22.4) | 57 (27.4) | 35 (17.2) | |
| EGFR mutation | 0.31 | |||
| Positive | 225 (54.7) | 120 (57.7) | 105 (51.7) | |
| Negative | 138 (33.6) | 66 (31.7) | 72 (35.5) | |
| Unknown | 48 (11.7) | 22 (10.6) | 26 (12.8) | |
Data are presented as n (%) or mean ± SD. GGO, ground-glass opacity; BMI, body mass index; CEA, carcinoembryonic antigen; MIP, micropapillary; EGFR, epidermal growth factor receptor; SD, standard deviation.
Effect of the GGO component on prognosis and recurrence pattern
In the entire cohort, the median follow-up time was 36 months [interquartile range (IQR), 11–107 months], and the 5-year RFS was 71.7% and 92.3% in the non-GGO group and the GGO group, respectively (P<0.001) (Figure S2A). Similarly, the 5-year CSS was 81.9% and 92.8% in the non-GGO group and the GGO group, respectively (P=0.02) (Figure S2B). Multivariate Cox analysis revealed that the GGO component [hazard ratio (HR) =0.232; 95% confidence interval (CI): 0.103–0.522; P<0.001] independently predicted RFS. Similarly, the GGO component (HR =0.397; 95% CI: 0.161–0.977; P=0.04) could independently predict the CSS of patients. Our survival analysis indicates that the tumor diameter, preoperative carcinoembryonic antigen levels is not a key prognostic factor for RFS or CSS in patients with pathological stage IA3 LUAD (Table S1).
Recurrence patterns significantly differed between the non-GGO and GGO groups in terms of ipsilateral lung metastases (5.3% vs. 0.5%, P=0.004), brain metastases (4.8% vs. 0.0%, P=0.002), and multiple organ metastases (1.9% vs. 0.0%, P=0.047). However, ipsilateral lymph node metastasis (1.4% vs. 0.0%, P=0.09), bone metastasis (0.5% vs. 1.5%, P=0.30), liver metastasis (1.0% vs. 1.0%, P=0.98), contralateral lung or lymph node metastasis (2.4% vs. 0.5%, P=0.11), and chest wall or pleural metastasis (1.4% vs. 0.0%, P=0.09) (Figure S3) were not significantly different between the groups.
Relevance of GGO to the prognosis and recurrence pattern of MIP-negative and MIP-positive status
In the GGO group, 168 patients (82.8%) had less than 5% MIP component, while 35 patients (17.2%) had more than 5% MIP. In the non-GGO group, 151 patients (72.6%) had less than 5% MIP, and 57 patients (27.4%) had more than 5% MIP. The results show that the proportion of MIP-positive patients is significantly higher in the GGO-negative group, with a statistically significant difference between the two groups (P<0.05) (Table 1). Furthermore, the prognostic relevance of the GGO component for patients depending on MIP-negative and MIP-positive status was evaluated. Our data revealed that the 5-year RFS (55.3% vs. 73.1%, P=0.08) (Figure 1A) and 5-year CSS (72.5% vs. 78.8%, P=0.95) (Figure 1B) were similar between the non-GGO and GGO groups among the MIP-positive patients. However, among the MIP-negative patients, the 5-year RFS was 78.6% and 96.4% in the non-GGO group and GGO group, respectively, while the 5-year CSS was 86.7% and 96.2% in the non-GGO group and GGO group, respectively. The RFS (P<0.001) (Figure 1C) and CSS (P=0.006) (Figure 1D) differed significantly between the groups. Multivariate analysis showed that the GGO component independently predicted RFS (HR =0.159; 95% CI: 0.047–0.541; P=0.003) and CSS (HR =0.202; 95% CI: 0.045–0.898; P=0.04) (Table 2) among the MIP-negative patients but was significantly associated with the prognosis of MIP-positive patients (Table S2).

Table 2
| Characteristics | RFS | CSS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariable | Multivariable | Univariable | Multivariable | ||||||||
| HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | ||||
| Sex | |||||||||||
| Female | |||||||||||
| Male | 4.459 (1.662–11.965) | 0.003 | 2.591 (0.792–8.470) | 0.12 | 7.192 (1.623–31.875) | 0.009 | 4.628 (0.885–24.195) | 0.07 | |||
| Age (years) | |||||||||||
| <65 | |||||||||||
| ≥65 | 1.667 (0.748–3.712) | 0.21 | 1.702 (0.650–4.455) | 0.28 | |||||||
| BMI (kg/m2) | 0.826 (0.710–0.960) | 0.01 | 0.837 (0.714–0.981) | 0.03 | 0.869 (0.723–1.045) | 0.14 | |||||
| Smoke history | |||||||||||
| No | |||||||||||
| Yes | 3.542 (1.578–7.951) | 0.002 | 1.426 (0.534–3.808) | 0.48 | 4.186 (1.579–11.095) | 0.004 | 1.685 (0.562–5.045) | 0.35 | |||
| Preoperative CEA (ng/mL) | |||||||||||
| <5 | |||||||||||
| ≥5 | 1.838 (0.826–4.093) | 0.14 | 1.294 (0.493–3.393) | 0.60 | |||||||
| Preoperative symptoms | |||||||||||
| No | |||||||||||
| Yes | 1.985 (0.889–4.435) | 0.09 | 1.030 (0.363–2.922) | 0.96 | |||||||
| Tumor size (cm) | 0.915 (0.166–5.051) | 0.92 | 0.800 (0.077–8.269) | 0.85 | |||||||
| Lymph node dissection | 0.954 (0.892–1.020) | 0.17 | |||||||||
| GGO component | |||||||||||
| Absence | |||||||||||
| Presence | 0.135 (0.40–0.453) | 0.001 | 0.159 (0.047–0.541) | 0.003 | 0.162 (0.037–0.714) | 0.02 | 0.202 (0.045–0.898) | 0.04 | |||
| EGFR mutation | |||||||||||
| Negative | |||||||||||
| Positive | 0.860 (0.371–1.993) | 0.73 | 1.494 (0.508–4.396) | 0.47 | |||||||
MIP, micropapillary; LUAD, lung adenocarcinoma; RFS, recurrence-free survival; CSS, cancer-specific survival; HR, hazard ratio; CI, confidence interval; BMI, body mass index; CEA, carcinoembryonic antigen; GGO, ground-glass opacity; EGFR, epidermal growth factor receptor.
In the MIP-positive patient cohort, while the 5-year RFS (55.3% vs. 73.1%, P=0.08) and 5-year CSS (72.5% vs. 78.8%, P=0.95) were similar between the GGO and non-GGO groups (Figure 1A,1B), short-term metastasis patterns showed differences. Specifically, the incidence of brain metastasis was 3.3% in the non-GGO group compared to 0.0% in the GGO group (P=0.02), and multiple organ metastases occurred in 2.6% of the non-GGO group compared to 0.0% in the GGO group (P=0.03) (Figure S4A). Among MIP-negative patients, the non-GGO group showed a higher incidence of ipsilateral lung metastasis (10.5% vs. 0.0%, P=0.047) and bone metastasis (0.0% vs. 8.6%, P=0.03) compared to the GGO group (Figure S4B). These findings highlight that although the short-term metastasis rates differ, this does not necessarily translate into significant long-term survival benefits in MIP-positive patients.
Association of GGO component with the survival of MIP-negative patients at 1, 2, and 3 years
The 1-year RFS was 82.5% and 96.9% in the non-GGO group and GGO group, respectively (Figure 2A), and the 2-year RFS was 85.9% in the non-GGO group and 96.9% in the GGO group (Figure 2B), respectively, with significant differences observed after 1 and 2 years of survival (1 year: P=0.002; 2 years: P=0.04). However, after 3 years of patient survival, no statistical difference in RFS was detected between the non-GGO and GGO groups (92.9% vs. 98.0%, P=0.40) (Figure 2C).

Similarly, the 1-year CSS was 87.3% in the non-GGO group and 96.2% in the GGO group (Figure 2D), and the 2-year CSS was 88.0% in the non-GGO group and 96.2% in the GGO group (Figure 2E), with significant differences after 1 and 2 years of survival (1 year: P=0.01; 2 years: P=0.02). The 3-year CSS was 92.5% in the non-GGO group and 97.1% in the non-GGO group, suggesting comparable rates (P=0.08) (Figure 2F).
Time-dependent multivariate analysis showed that GGO components were independent predictors of 1-year RFS (HR =0.178; 95% CI: 0.040–0.787; P=0.02) and 2-year RFS (HR =0.196; 95% CI: 0.044–0.874; P=0.03) but not 3-year RFS (HR =0.189; 95% CI: 0.023–1.524; P=0.12). Similarly, GGO components were independent predictors of 1-year CSS (HR =0.118; 95% CI: 0.027–0.521; P=0.005) and 2-year CSS (HR =0.197; 95% CI: 0.042–0.923; P=0.04) but not 3-year CSS (HR =0.310; 95% CI: 0.031–3.082; P=0.32) (Figure 3).

Dynamic recurrence events in the pathological stage IA3 LUAD subgroups
To investigate the impact of MIP components and GGO on the prognosis of pathological stage IA3 LUAD, patients were classified into four subgroups based on the presence or absence of MIP and GGO: MIP(+)/GGO(+), MIP(+)/GGO(−), MIP(−)/GGO(+), and MIP(−)/GGO(−). The life-table method was employed to calculate the monthly recurrence probability for each subgroup.
The recurrence risk was relatively high in the MIP(+)/GGO(+) and MIP(+)/GGO(−) subgroups, with peak recurrence occurring at 44 and 43 months postoperatively, respectively (Figure 4A,4B). In contrast, the MIP(−)/GGO(+) subgroup exhibited a comparatively lower recurrence risk, which peaked at 44 months (Figure 4C). However, in the MIP(−)/GGO(−) subgroup, although the peak recurrence risk occurred later, at 54 months, it remained noteworthy and requires continued surveillance due to the sustained risk of recurrence (Figure 4D).

Individualized follow-up strategy for patients with pathological stage IA3 LUAD
The follow-up schedule recommended by the NCCN guidelines for patients with pathological stage IA3 LUAD is displayed in Figure 5, with eight follow-up sessions over 5 years being recommended. Based on the different risks of recurrence among patients in different subgroups, we proposed a follow-up strategy that considers the risk of recurrence for each month. The recommended follow-up session for the MIP(+)-GGO(+), MIP(+)-GGO(−), MIP(−)-GGO(+), and MIP(−)-GGO(−) subgroups over 5 years were 3, 9, 3, and 11, respectively. For instance, for patients with pathological stage IA3 LUAD and MIP(+)-GGO(+) status, follow-up was recommended at 29, 40, and 44 months postoperatively.
Discussion
This study evaluated the predictive significance of the GGO component in MIP-positive and MIP-negative patients with pathological stage IA3 LUAD undergoing lobectomy and its implications for tailoring personalized postoperative monitoring approaches. The results showed that GGO was associated with improved RFS and CSS, particularly in MIP-negative patients. Time-dependent Cox multivariate analysis demonstrated that GGO was an effective prognostic factor for MIP-negative patients for up to 2 years postoperatively. Furthermore, MIP and GGO components were used to subgroup patients, and a monitoring strategy that considers the probability of postoperative recurrence was devised. The recommended number of follow-up sessions for the MIP(+)-GGO(+), MIP(+)-GGO(−), MIP(−)-GGO(+), and MIP(−)-GGO(−) subgroups over 5 years were 3, 9, 3, and 11, respectively.
Several previous studies have demonstrated that patients with early LUAD with a GGO component have a more favorable prognosis compared to those without a GGO component (19-21). Radiologically, the presence of a GGO component corresponds to a noninvasive lepidic growth pattern observed in pathological tissue (22). However, whether a GGO component has favorable prognostic value for pathological stage IA3 LUAD has not been conclusively established. The multicenter data from our study suggest that the presence of a GGO component is associated with prolonged RFS and CSS. Previous research indicates that solid LUAD, compared to LUAD with a GGO component, is more likely to lead to ipsilateral lung and brain metastases (18). Likewise, our findings demonstrated a significant reduction in the risk of ipsilateral lung metastasis and brain metastases associated with the presence of a GGO component.
It has been previously suggested that the presence of an MIP component renders lung cancer cells resistant to apoptosis and is thus associated with a high frequency of micrometastasis and an increased risk of recurrence (10,23,24). Our subgroup analysis revealed that the presence of a GGO component was only associated with the prognosis of MIP-negative but not MIP-positive patients. This suggests that while the presence of a GGO component positively influences prognosis, it may not sufficiently counteract the negative impact of MIP-positive status on tumor invasiveness. Prior studies have also indicated that the predictive value of known prognostic factors for patients with cancer is not consistent with extended survival time (25,26). In this study, the GGO component was a significant prognostic factor for favorable postoperative outcomes in MIP-negative patients within 2 years, but the predictive value was lost after 3 years of survival.
A dynamic recurrence curve provides detailed information on recurrence time and risk, serving as a valuable reference for clinical follow-up planning (27-30). The NCCN does not provide separate follow-up recommendations for patients with pathological stage IA3 LUAD (17). However, our stratification of patients into MIP(+)-GGO(+), MIP(+)-GGO(−), MIP(−)-GGO(+), and MIP(−)-GGO(−) subgroups revealed significant differences in recurrence timing and risk between subgroups, suggesting that recurrence does not follow a regular interval. Consequently, we developed an individualized follow-up schedule, in which the recommended number of follow-up sessions for the MIP(+)-GGO(+), MIP(+)-GGO(−), MIP(−)-GGO(+), and MIP(−)-GGO(−) subgroups over 5 years were 3, 9, 3, and 11, respectively.
This study also involved several limitations which should be acknowledged. First, despite the inclusion of patients with pathological stage IA3 LUAD from four institutions, the proportion of MIP-positive patients remained relatively low, at about 22.4% (92/411). Larger sample sizes from multiple centers and prospectively designed studies are needed. Second, there is no global consensus concerning which is approach is best suited to assessing GGO composition; moreover, our study was conducted on a Chinese population, and thus our findings may not be generalizable to Western populations. Nevertheless, our study demonstrated that the GGO component is associated with the RFS and CSS of MIP-negative patients with pathological stage IA3 LUAD, and we have accordingly proposed personalized follow-up strategies based on monthly recurrence risk.
Conclusions
The presence of a GGO component was associated with prolonged RFS and CSS in MIP-negative patients with pathological stage IA3 LUAD but was not associated with a significantly improved prognosis in MIP-positive patients. Moreover, correlation of GGO with recurrence patterns differed between the MIP-positive and MIP-negative patients. GGO and MIP components and their respective pathological characteristics are the basis of distinct subgroups of patients that may have unique recurrence risks and timing profiles. The follow-up strategy based on the dynamic recurrence curve is more personalized and may provide valuable guidance for clinical practice.
Acknowledgments
Funding: This study was supported by grants from
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-923/rc
Data Sharing Statement: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-923/dss
Peer Review File: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-923/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-923/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of the Fujian Medical University Union Hospital (IRB No. 2023KY190). All participating hospitals were informed and agreed with this study. The requirement for patients’ informed consent was waived as it was a retrospective research.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ito H, Suzuki K, Mizutani T, et al. Long-term survival outcome after lobectomy in patients with clinical T1 N0 lung cancer. J Thorac Cardiovasc Surg 2020; Epub ahead of print. [Crossref] [PubMed]
- Suzuki K, Saji H, Aokage K, et al. Comparison of pulmonary segmentectomy and lobectomy: Safety results of a randomized trial. J Thorac Cardiovasc Surg 2019;158:895-907. [Crossref] [PubMed]
- Ye T, Deng L, Wang S, et al. Lung Adenocarcinomas Manifesting as Radiological Part-Solid Nodules Define a Special Clinical Subtype. J Thorac Oncol 2019;14:617-27. [Crossref] [PubMed]
- Asamura H, Hishida T, Suzuki K, et al. Radiographically determined noninvasive adenocarcinoma of the lung: survival outcomes of Japan Clinical Oncology Group 0201. J Thorac Cardiovasc Surg 2013;146:24-30. [Crossref] [PubMed]
- Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244-85. [Crossref] [PubMed]
- Travis WD, Brambilla E, Noguchi M, et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society: international multidisciplinary classification of lung adenocarcinoma: executive summary. Proc Am Thorac Soc 2011;8:381-5. [Crossref] [PubMed]
- Cha MJ, Lee HY, Lee KS, et al. Micropapillary and solid subtypes of invasive lung adenocarcinoma: clinical predictors of histopathology and outcome. J Thorac Cardiovasc Surg 2014;147:921-928.e2. [Crossref] [PubMed]
- Xu SJ, Tu JH, Chen H, et al. A Multi-institutional Analysis of the Combined Effect of Micropapillary Component and Consolidation-to-Tumor Ratio >0.5 on the Prognosis of Pathological, Stage IA3, Lung Adenocarcinoma. Ann Surg Oncol 2023;30:5843-53. [Crossref] [PubMed]
- Mikubo M, Tamagawa S, Kondo Y, et al. Micropapillary and solid components as high-grade patterns in IASLC grading system of lung adenocarcinoma: Clinical implications and management. Lung Cancer 2024;187:107445. [Crossref] [PubMed]
- Watanabe K, Sakamaki K, Ito H, et al. Impact of the micropapillary component on the timing of recurrence in patients with resected lung adenocarcinoma. Eur J Cardiothorac Surg 2020;58:1010-8. [Crossref] [PubMed]
- Tsubokawa N, Mimae T, Sasada S, et al. Negative prognostic influence of micropapillary pattern in stage IA lung adenocarcinoma. Eur J Cardiothorac Surg 2016;49:293-9. [Crossref] [PubMed]
- Bai J, Fu F, Sun W, et al. Prognostic effect of ground-glass opacity in subcentimeter invasive lung adenocarcinoma. J Thorac Dis 2023;15:1559-71. [Crossref] [PubMed]
- Zhu W, Bai N, Cao J, et al. Genetic characteristics of lung adenocarcinoma with ground-glass opacity component. J Thorac Dis 2023;15:6106-14. [Crossref] [PubMed]
- Kim H, Goo JM, Kim YT, et al. Validation of the Eighth Edition Clinical T Categorization System for Clinical Stage IA, Resected Lung Adenocarcinomas: Prognostic Implications of the Ground-Glass Opacity Component. J Thorac Oncol 2020;15:580-8.
- Kamigaichi A, Tsutani Y, Mimae T, et al. The prognostic impact of the ground-glass opacity component in nearly pure-solid stage IA non-small-cell lung cancer. Eur J Cardiothorac Surg 2022;62:ezac166. [Crossref] [PubMed]
- Miyoshi T, Aokage K, Katsumata S, et al. Ground-Glass Opacity Is a Strong Prognosticator for Pathologic Stage IA Lung Adenocarcinoma. Ann Thorac Surg 2019;108:249-55. [Crossref] [PubMed]
- Ettinger DS, Wood DE, Aisner DL, et al. Non-Small Cell Lung Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2022;20:497-530. [Crossref] [PubMed]
- Park S, Lee SM, Choe J, et al. Recurrence Patterns and Patient Outcomes in Resected Lung Adenocarcinoma Differ according to Ground-Glass Opacity at CT. Radiology 2023;307:e222422. [Crossref] [PubMed]
- Xu SJ, Chen RQ, Tu JH, et al. Effects of a ground-glass opacity component on the recurrence and survival of pathological stage IA3 lung adenocarcinoma: a multi-institutional retrospective study. Transl Lung Cancer Res 2023;12:1078-92. [Crossref] [PubMed]
- Huang KX, Gibney BC. Pure ground-glass opacities (GGO) lung adenocarcinoma: surgical resection is curative. J Thorac Dis 2024;16:3518-21. [Crossref] [PubMed]
- Ma Z, Zhang Y, Han H, et al. Segmentectomy versus lobectomy for ground-glass opacity dominant cT1N0 invasive lung adenocarcinoma. Transl Lung Cancer Res 2024;13:1201-9. [Crossref] [PubMed]
- Hattori A, Matsunaga T, Takamochi K, et al. Importance of Ground Glass Opacity Component in Clinical Stage IA Radiologic Invasive Lung Cancer. Ann Thorac Surg 2017;104:313-20. [Crossref] [PubMed]
- Zhao Y, Wang R, Shen X, et al. Minor Components of Micropapillary and Solid Subtypes in Lung Adenocarcinoma are Predictors of Lymph Node Metastasis and Poor Prognosis. Ann Surg Oncol 2016;23:2099-105. [Crossref] [PubMed]
- Tsao MS, Marguet S, Le Teuff G, et al. Subtype Classification of Lung Adenocarcinoma Predicts Benefit From Adjuvant Chemotherapy in Patients Undergoing Complete Resection. J Clin Oncol 2015;33:3439-46. [Crossref] [PubMed]
- Xu SJ, Chen C, Tu JH, et al. Dynamic Analysis of the Impact of Micropapillary Component on Different Recurrence Patterns of Pathological Stage IA3 Lung Adenocarcinoma: A Multicenter, Retrospective Study. Ann Surg Oncol 2024;31:872-82. [Crossref] [PubMed]
- Chen QY, Zhong Q, Wang W, et al. Prognosis of Young Survivors of Gastric Cancer in China and the U.S.: Determining Long-Term Outcomes Based on Conditional Survival. Oncologist 2019;24:e260-74. [Crossref] [PubMed]
- Watanabe K, Tsuboi M, Sakamaki K, et al. Postoperative follow-up strategy based on recurrence dynamics for non-small-cell lung cancer. Eur J Cardiothorac Surg 2016;49:1624-31. [Crossref] [PubMed]
- Yun JK, Lee GD, Choi S, et al. Various recurrence dynamics for non-small cell lung cancer depending on pathological stage and histology after surgical resection. Transl Lung Cancer Res 2022;11:1327-36. [Crossref] [PubMed]
- Schmidt-Hansen M, Baldwin DR, Hasler E. What is the most effective follow-up model for lung cancer patients? A systematic review. J Thorac Oncol 2012;7:821-4. [Crossref] [PubMed]
- Xu BB, He XY, Zhou YB, et al. Optimal postoperative surveillance strategies for cancer survivors with gastric neuroendocrine carcinoma based on individual risk: a multicenter real-world cohort study. Int J Surg 2023;109:1668-76. [Crossref] [PubMed]
(English Language Editor: J. Gray)


